Assessing
Your Progress
The
lefts
for Medicare
&
Medicaid
Services
(CMS)
has released
a
new
infographic based
on the
Next
Steps
Toolkit
to
help you
analyze
your ICD-10
progress.
By tracking
and comparing
key performance
indicators,
you can
assess
your progress,
address
your findings,
and maintain
your progress.
Today,
we will
explore
how to
assess
your progress.
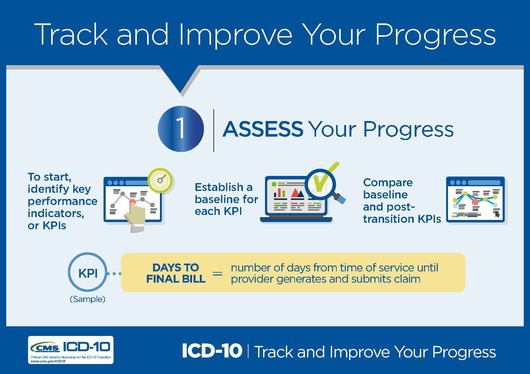
Establish
a Baseline
for Each
Key Performance
Indicator
The
first
step in
using
key
performance
indicators (KPIs)
is establishing
a point
of comparison
for each
KPI you
would
like to
track.
Your goal
should
be to
compare
KPIs from
before
and after
the October
1, 2015,
transition
date.
Using
KPIs
CMS
has released
a
companion
resource focusing
on KPIs
to help
you better
understand
how to
assess
your ICD-10
progress.
This fact
sheet
includes
a list
of KPIs
that may
be helpful
to your
practice.
If
you’re
a provider
in a small
practice,
you might
not have
routinely
used or
tracked
KPIs in
the past.
You may
need to
start
by developing
a new
baseline
with current
data.
Work with
your billing
and coding
staff
to see
what data
are already
available
in your
systems,
reports,
and records.
You can
also check
if pre-ICD-10
data is
available
from outside
sources
like:
Clearinghouses Third-party
billers System
vendors
Keep
Up to
Date on
ICD-10
Visit
the CMS ICD-10
website and Roadto10.org for
the latest
news and
official
resources,
including
the Next
Steps
Toolkit, ICD-10
Quick
Start
Guide, and
a contact
list for
provider
Medicare
and Medicaid
questions.
Sign up
for CMS
ICD-10
Email
Updates and follow
us on
Twitter.
|