
Billing Instructions: Acceptable Claims, ctm5010 14a
Attachments and ASC X12N 835 v.5010 Transactions
5/20/2016
A new requirement for OB Patients for Global Billing requires providers to now include 13 ante partum visits on the HCFA 1500, whether sent on paper or electronically:
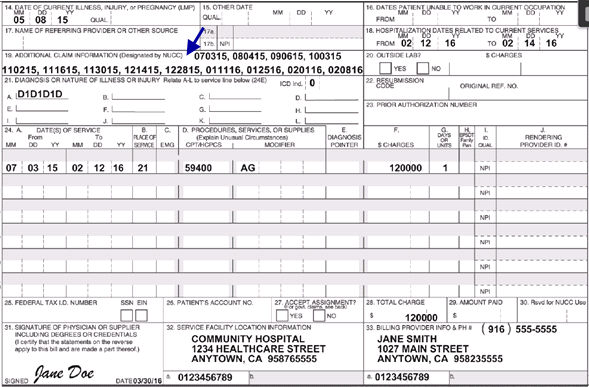
Electronic Claims need to be sent with a PWK/NTE with an Attachment Control Number (ACN) that is from an Attachment Control Form (ACF) published by MCAL.
Add the ACN from the form in the Charge Remark, then fax the information to MCAL.
Supporting Documentation –
Notes
Certain Medi-Cal claims require supporting documentation thatcan be noted in the Remarks field/Additional Claim Information field
(Box 19) of the paper claim. These claims also are acceptable for CMC submission and require using the ASC X12N 837 v.5010 Note (NTE) Segments.
The following list represents some of the circumstances under which claims may be submitted through CMC with appropriate substantiating statements in the ASC X12N 837 v.5010 Note (NTE) Segments.
· When billing with certain HCPCS or CPT-4 codes, including:
Unlisted Include procedure description and price in
Procedures the ASC X12N 837 v.5010 Note (NTE) Segments.
Unlisted Include name of drug, strength, dosage
Injections and invoice cost in the ASC X12N 837 v.5010 Note (NTE) Segments.
“By Report” Include additional clinical information or
Procedures report in the ASC X12N 837 v.5010 Note (NTE) Segments.
Unusual/ Include complicating or unusual
Complicated circumstances in Procedures ASC X12N 837 v.5010 Note (NTE) Segments.
· When billing with multiple or “By Report” modifiers (for example, -99, -51, -22).
· When submitting claims using delay reason codes 1, 3 – 6 or 11 for the ASC X12N 837 v.5010 format.
· When submitting claims requiring a Medi-Services Request obtained through the POS network or AEVS.
· When submitting claims for Medicare non-covered services.
· When billing for a newborn using the mother’s Medi-Cal identification number.
· When including an emergency statement.
· When billing for compounded prescriptions (except TPN).
· When submitting Long Term Care claims detailing Share of Cost expenditures.
Supporting Documentation –
Attachments
Certain Medi-Cal claims require supporting documentation that cannot be noted in the Remarks field/Additional Claim Information field.
(Box 19) but must be submitted as an attachment. These claims can be submitted electronically using the ASC X12N 837 v.5010 claim file format. There are three methods for sending in attachments with a claim:
· Paper attachments can be mailed to Medi-Cal with an Attachment Control Form (ACF) cover sheet. The ACF contains an Attachment Control Number (ACN) used to link the attachment to its respective electronic claim. The ACN must be entered in the ASC X12N 837 v.5010 Paperwork (PWK) Segments.
· Faxed attachments can be sent to Medi-Cal with the ACF as a cover sheet and the ACN that links the attachment to its respective electronic claim. The ACN from the corresponding ACF must be entered in the ASC X12N 837 v.5010 Paperwork (PWK) Segments. Each fax must be sent separately and must include one ACF followed by the corresponding pages of the attachment. The fax number is 1-866-438-9377.
Electronic attachments can be sent to Medi-Cal by an approved third-party vendor who will preprocess the attachments and submit them on behalf of the provider. For electronic attachment submissions, the ACN will be supplied to the provider by the vendor and must be entered in the ASC X12N 837 v.5010 Paperwork (PWK) Segments. Contact information for electronic attachment vendors can be found on the Medi-Cal website in the CMC Developers, Vendors and Billing Services Directory
Examples of claims submitted through CMC with separate attachments include:
· Claims that require an Explanation of Medicare Benefits, Medicare Remittance Notice or Remittance Advice (Medicare status codes 1 – 7 and 9).
· Claims that include denials from other health coverage carriers such as CHAMPUS, Kaiser, Ross Loos or prepaid health plans.
· Claims billing HCPCS or CPT-4 codes where the price is not listed with Medi-Cal.
· The submitter is unable to include the pricing information for the ASC X12N 837 v.5010 Note (NTE) Segment.
· Claims requiring sterilization or hysterectomy consent forms.
Attachment Control Form: Required and Optional Fields
1. The Provider Number is a required field and must be clearly printed in the box provided.
2. The Provider Name is an optional field, but is recommended for purposes of timely communication with the submitter, if needed.
3. The Provider Address is an optional field, but is recommended for purposes of timely communication with the submitter, if needed.
4. The Provider Signature is a required field that must be completed by the provider.
5. Forms and attachments can be mailed to the address shown on the Attachment Control Form (ACF) or faxed to 1-866-438-9377. Each fax must include an ACF as the cover page followed by the corresponding attachment pages. Additional ACFs and attachments must be faxed separately.
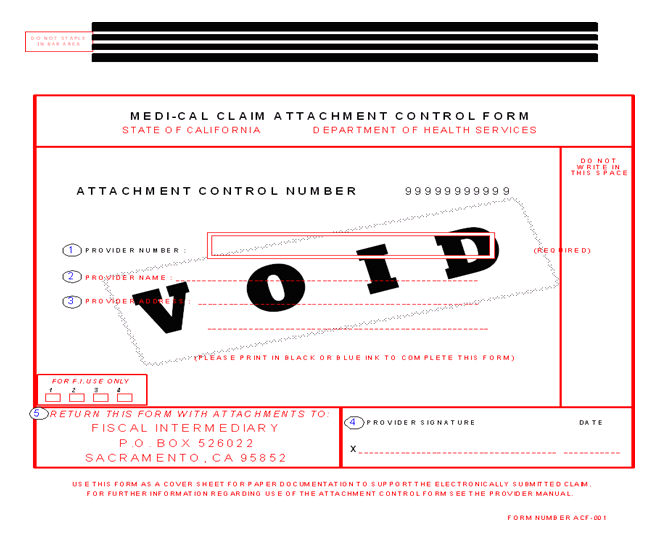
Attachment Control Form (ACF) The ACF must be an original form obtained from Medi-Cal. Copies of
Guidelines the ACF will not be accepted.
The DHCS Fiscal Intermediary (FI) must receive the ACF and attachments within 30 days after or before the electronic claim submission date. See example below.
The 30-day “window” is based on the day the attachment or claim is received by the Fiscal Intermediary (FI). Medi-Cal is not responsible for any postal delays in receiving the attachments.
The following example illustrates the time frame limitations for accepting attachments for claims.
In this example, the Provider submits four claims, which are received over a period of 61 days. All four claims require the same attachments.
Day 1: Claim A received. ACF and attachments for Claim A must be received by Day 30.
Day 2: Claim B received. ACF and attachments for Claim B must be received by Day 31.
Day 31: ACF/Attachment 1 received. Since it was received more than 30 days after Claim A, Claim A will be denied. It can be matched to Claim B, since it was received within 30 days of Claim B.
Day 60: Claim C received. Since it was received within 30 days of ACF/Attachment 1, the attachments can be matched to Claim C.
Day 61: Claim D received. Since this is more than 30 days after ACF/Attachment 1 was received, the attachments cannot be matched to Claim D, which will be denied.
Note: In the example above, Claims A, B, C and D could be different claims, or these four claims could include resubmissions of the same claim. In either case, all of the claims could use the same Attachment Control Number (ACN).