CMS-1500
Claim Form Instructions
February 2008
NHIC, Corp.
MEDICARE
CMS-1500 Claim Form Instructions
________________________________________________________________________
TABLE OF CONTENTS
Introduction.....................................................................................................................................3
Preparing the CMS-1500 claim form...............................................................................................4
The Form CMS-1500-(08-05) .........................................................................................................6
Instructions for Filling Out the Health Insurance Claim Form-1500 ..............................................10
Appendix A – Sample Wording For Authorizations.......................................................................30
Appendix B - Place of Service Codes with Definitions..................................................................31
Telephone and Address Directory ................................................................................................37
Mailing Address Directory.............................................................................................................38
Internet Resources .......................................................................................................................42 NHIC, Corp. 2 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
INTRODUCTION
The Provider Education and Outreach Team at NHIC, Corp. developed this guide to provide you with Medicare Part B CMS-1500 Claim Form Instructions. It is intended to serve as a useful supplement to other manuals published by NHIC, and not a replacement. The information provided in no way represents a guarantee of payment. Benefits for all claims will be based on the patient's eligibility, provisions of the Law, and regulations and instructions from Centers for Medicare & Medicaid Services (CMS). It is the responsibility of each provider or practitioner submitting claims to become familiar with Medicare coverage and requirements. All information is subject to change as federal regulations and Medicare Part B policy guidelines, mandated by the Centers for Medicare & Medicaid Services (CMS), are revised or implemented.
This information guide, in conjunction with the NHIC website (www.medicarenhic.com), Medicare B Resource (quarterly provider newsletter), and special program mailings, provide qualified reference resources. We advise you to check our website for updates to this guide. To receive program updates, you may join our mailing list by clicking on “Join Our Mailing List” on our website. Most of the information in this guide is based on Publication 100-04, Chapter 26 of the CMS Internet Only Manual (IOM). The CMS IOM provides detailed regulations and coverage guidelines of the Medicare program. To access the manual, visit the CMS website at http://www.cms.hhs.gov/manuals/
DISCLAIMER: This information release is the property of NHIC, Corp. It may be freely distributed in its entirety but may not be modified, sold for profit or used in commercial documents. The information is provided “as is” without any expressed or implied warranty. While all information in this document is believed to be correct at the time of writing, this document is for educational purposes only and does not purport to provide legal advice. All models, methodologies and guidelines are undergoing continuous improvement and modification by NHIC, Corp. and the Centers for Medicare & Medicaid Services (CMS). The most current edition of the information contained in this release can be found on the NHIC, Corp. web site at www.medicarenhic.com and the CMS web site at www.cms.hhs.gov. The identification of an organization or product in this information does not imply any form of endorsement.
If you have questions or comments regarding this material, please call the appropriate NHIC Customer Service Center for your state. The telephone numbers are listed at the end of this guide. The CPT codes, descriptors, and other data only are copyright 2007 by the American Medical Association. All rights reserved. Applicable FARS/DFARS apply. The ICD-9-CM codes and their descriptors used in this publication are copyright 2007 under the Uniform Copyright Convention. All rights reserved. Current Dental Terminology, fourth edition (CDT-4) (including procedure codes, definitions (descriptions) and other data) is copyrighted by the American Dental Association. © 2006 American Dental Association. All rights reserved. Applicable FARS/DFARS apply.
NHIC, Corp. 3 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
PREPARING THE CMS-1500 CLAIM FORM
The Form CMS-1500 (Health Insurance Claim Form) is the standard claim form used by a non-institutional provider or supplier to bill Medicare contractors and durable medical equipment contractors when a provider qualifies for a waiver from the Administrative Simplification Compliance Act (ASCA) requirement for electronic submission of claims.
The National Uniform Claim Committee (NUCC) is responsible for the maintenance of the form CMS-1500. CMS and contractors do not provide the form to providers for claim submission. Forms may be purchased from the U.S. Government Printing Office at (866) 512-1800, local printing companies in your area and/or office supply stores. Each of these sources sells the Health Insurance Claim Form CMS-1500 in various configurations (single part, multi-part, continuous feed, laser, etc.)
NUCC revised the Form CMS-1500. The new version, Form CMS-1500 (08-05) replaced the CMS-1500 (12-90) version. The 08-05 version of the CMS-1500 form was effective June 29, 2007. Medicare will reject any 12-90 version forms received.
For more information, please visit the CMS website at:
http://www.cms.hhs.gov/ElectronicBillingEDITrans/16_1500.asp
Intelligent Character Recognition (ICR)
NHIC is using an Intelligent Character Recognition (ICR) system to capture claims information directly from the CMS-1500 claim form.
ICR benefits include:
Greater efficiency;
Improved accuracy;
More control over the data input, and
Reduced data entry cost for the Medicare program.
The ICR is capable of going beyond simply scanning claims data into the computer and has a sophisticated computer “brain” which verifies claims information against several data files as well as performing various claims processing functions.
With the ICR system, it is important that claims be submitted with proper and legible coding. This is because the ICR output is largely dependent on the accuracy and legibility of the claim form submitted.
If you are not billing electronically, consider it! However, when you bill on paper, follow these tips when completing your CMS-1500 forms:
NHIC, Corp. 4 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
The font should be:
Legible (Change typewriter ribbon/PC printer cartridge frequently, if necessary. Laser printers are
recommended)
In Black Ink
Pica, Arial 10, 11 or 12 font type
CAPITAL letters
The font must NOT have:
Broken characters
Script, Italics or Stylized font
Red ink
Mini-font
Dot Matrix font
Do NOT bill with:
Liquid correction fluid changes.
Data touching box edges or running outside of numbered boxes (left justify information in each box).
Exception: when using the 8-digit date format, information may be typed over the dotted lines shown in date fields, i.e., Item 24a.
More than six service lines per claim (use a new form for additional services);
Narrative descriptions of procedure, narrative description of modifier or narrative description of
diagnosis (the CPT, Modifier or ICD-9-CM codes are sufficient);
Stickers or rubber stamps (such as “tracer,” “corrected billing,” provider name and address, etc.);
NHIC's address at top of the form;
Special characters (i.e., hyphens, periods, parentheses, dollar signs and ditto marks).
Handwritten descriptions;
Attachments smaller than 8 1/2 x 11.
The claim form must be:
An original CMS-1500 printed in red “drop out “ ink with the printed information on back (photocopies
are not acceptable);
Size - 8½ ” x 11” with the printer pin-feed edges removed at the perforations;
Free from crumples, tears, or excessive creases (to avoid this, submit claims in an envelope that is full
letter size or larger);
Thick enough (20-22 lbs.) to keep information on the back from showing through;
Clean and free from stains, tear-off pad glue, notations, circles or scribbles, strike-overs, crossed-out
information or white out.
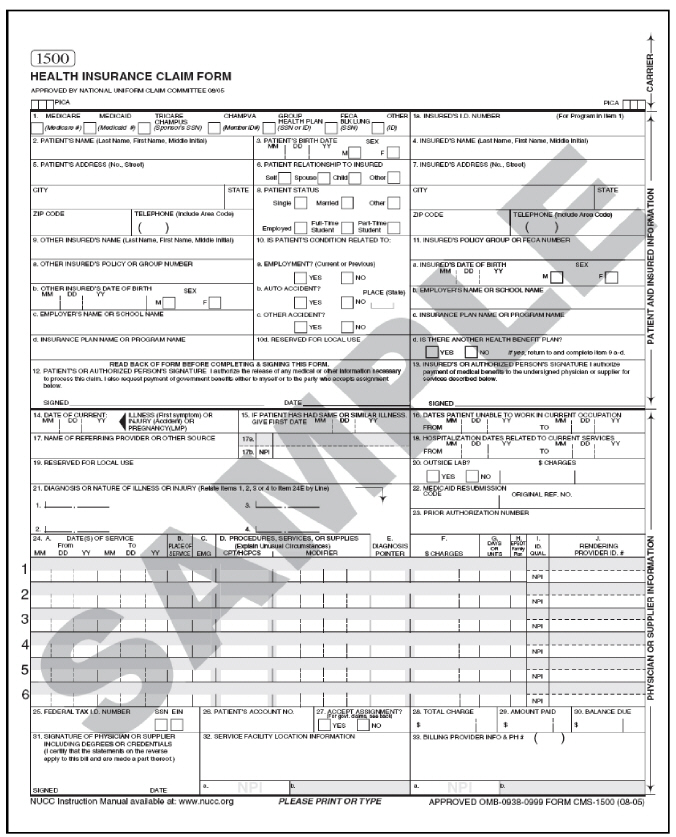
NOTE: The following examples are in black and white. An original CMS-1500 claim form is printed in red “drop out” ink with the printed information on the back.
NHIC, Corp. 5 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
THE FORM CMS-1500-(08-05)
The Form CMS-1500 answers the need of many health insurers. It is the basic form prescribed by CMS for the Medicare program and is only accepted from physicians and suppliers that are excluded from the mandatory electronic submission requirement. The instructions for completion of the paper claim form provide required and conditional elements that are also applicable to electronic billing. Consult your Medicare-specific Companion Document to the Implementation Guide for Health Care Claim Professional 837 for assistance with electronic billing.
Providers and suppliers must report 8-digit dates in all date of birth fields (items 3, 9b, and 11a), and either 6-digit or 8-digit dates in all other fields (items 11b, 12, 14, 16, 18, 19, 24a, and 31).
Providers of service and suppliers have the option of entering 6 or 8-digit dates in items 11b, 14, 16, 18, 19, or 24a. However, if a provider of service or supplier chooses to enter 8-digit dates for items 11b, 14, 16, 18, 19, or 24a, he or she must enter 8-digit dates for all these fields. For instance, a provider or supplier will not be permitted to enter 8-digit dates for items 11b, 14, 16, 18, 19, and a 6-digit date for item 24a. The same applies to providers and suppliers who choose to submit 6-digit dates. Items 12 and 31 are exempt from this requirement.
Mandatory Reporting of the NPI on all Part B Claims
Effective March, 1, 2008, your Medicare fee-for-service claims must include an NPI in the primary provider fields on the claim (i.e.; the billing, pay-to-provider, and rendering provider fields). You may continue to submit NPI/legacy pairs in these fields or submit only your NPI. The secondary provider fields (i.e.; referring, ordering, and supervising) may continue to include only your legacy number, if you choose. Failure to submit an NPI in the primary provider identifier fields will result in your claims being rejected.
As of May 23, 2008, all claims must be submitted with NPI only in all primary and secondary fields. Claims containing legacy numbers will be rejected.
NHIC, Corp. 6 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
NHIC, Corp. 7 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.

NHIC, Corp. 8 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
INSTRUCTIONS FOR FILLING OUT THE HEALTH INSURANCE CLAIM
FORM-1500
CONTRACTOR NOTE: Items marked with “R” (Required) or “C” (Conditionally Required) will cause your claim to be rejected if they are missing, invalid, or incomplete. However, there are many other items on the claim form which must be properly completed, or your claim will be developed, delayed or denied.
Publications (Pub.) referenced in the instructions refer to the CMS Internet Only Manual (IOM).
Reminder: For date fields other than date of birth, all fields shall be one or the other format, 6-digit: (MM/DD/YY) or 8-digit: (MM/DD/CCYY). Intermixing the two formats on the claim is not allowed.
|
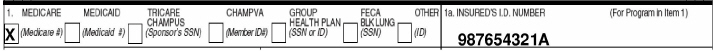
Item 1: |
Show the type of health insurance coverage applicable to this claim by checking the CONTRACTOR NOTE: Do not use dashes in number. Be sure to add the letter suffix. |
|
|
Item 1a: |
|
Enter the patient's Medicare Health Insurance Claim Number (HICN) whether Medicare is |
ANYWHERE CA
56789 111 555-1212
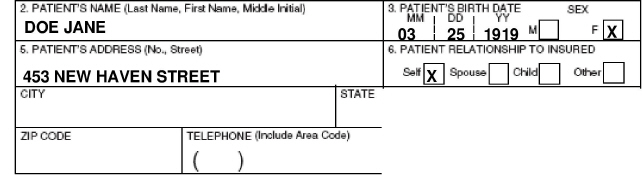
Illustration for Items 2 though 6.
|
Item 2: |
Enter the patient's last name, first name, and middle initial, if any, as shown on the |
|
Item 3: |
Enter the patient's 8-digit birth date (MM/DD/CCYY) and sex. |
|
Item 4: |
If there is insurance primary to Medicare, either through the patient's or spouse's |
NHIC, Corp. 10 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
|
Item 5: |
Enter the patient's mailing address and telephone number. On the first line enter the street |
||
|
Item 6: |
Check the appropriate box for patient's relationship to insured when item 4 is completed. |
||
|
Item 7: |
|
Enter the insured's address and telephone number. When the address is the same as the |
|
|
Item 8: |
Check the appropriate box for the patient's marital status and whether employed or a |
||
|
|
|
|
|
|
Item 9: |
Enter the last name, first name, and middle initial of the enrollee in a Medigap policy if it is NOTE: Only participating physicians and suppliers are to complete Item 9 and its Participating physicians and suppliers must enter information required in item 9 and its Medigap – A Medigap policy meets the statutory definition of a “Medicare supplemental |
||
NHIC, Corp. 11 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
|
|
|
“specified disease” or “hospital indemnity” coverage. Also, it explicitly excludes a policy or Do not list other supplemental coverage in item 9 and its subdivisions at the time a Medicare |
|
|
|
|
03 25 1919 X 123456789
|
|
|
|
|
Illustration for Items 9 though 9d. |
|
|
Item 9a: |
|
Enter the policy and/or group number of the Medigap insured preceded by MEDIGAP, MG, or |
|
NOTE: Item 9d must be completed, even when the provider enters a policy and/or group number in Item 9a.
|
Item 9b: |
|
Enter the Medigap insured's 8-digit birth date (MM/DD/CCYY) and sex. |
|
Item 9c: |
|
Leave blank if a Medigap PAYERID is entered item 9d. Otherwise, enter the claims |
For example:
1257 Anywhere Street
Baltimore, MD 21204
is shown as “1257 ANYWHERE ST MD 21204.”
|
Item 9d: |
|
Enter in the 9-digit PAYERID number of the Medigap insurer. If no PAYERID number exists, |
If the Medicare beneficiary wants Medicare payment data forwarded to a Medigap insurer through the Medigap claim-based crossover process, the participating provider of service or
NHIC, Corp. 12 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
supplier must accurately complete all of the information in items 9, 9a, 9b, and 9d. A Medicare participating provider or supplier shall only enter the COBA Medigap claim-based ID within item 9d when seeking to have the beneficiary's claim crossed over to a Medigap insurer. If a participating provider or supplier enters the PAYERID or the Medigap insurer program or its plan name within item 9d, the Medicare Part B contractor will be unable to forward the claim information to the Coordinator of Benefits Contractor.
CONTRACTOR NOTE : The Medigap claim-based IDs that fall in the range of 55000 through 59999 can be found on the CMS website at
http://www.cms.hhs.gov/COBAgreement/Downloads/Medigap%20Claim-based%20COBA%20IDs%20for%20Billing%20Purpose.pdf
|
Item 10a-c: |
Check “YES” or “NO” to indicate whether employment, auto liability, or other accident |
|
Item 10d: |
|
|
Item 11: |
THIS ITEM MUST BE COMPLETED, IT IS A REQUIRED FIELD. BY COMPLETING THIS |
NHIC, Corp. 13 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
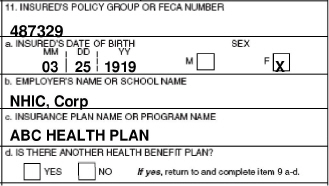
Illustration for item 11 through 11d.
If there is insurance primary to Medicare, enter the insured's policy or group number and
proceed to items 11a-11c. Items 4, 6, and 7 must also be completed.
NOTE: Enter the appropriate information in item 11c if insurance primary to Medicare is
indicated in item 11.
If there is no insurance primary to Medicare, enter the word “NONE” and then proceed to
item 12.
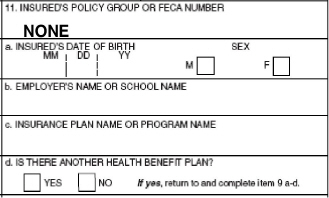
If the insured reports a terminating event with regard to insurance which had been primary
to Medicare (e.g., insured retired), enter the word “NONE,” and proceed to item 11b.
If a lab has previously collected and retained MSP information for a beneficiary, the lab may
use that information for billing purposes of the non-face-to-face lab service. If the lab has no
MSP information for the beneficiary, the lab will enter the word “None” in item 11 of Form
CMS-1500, when submitting a claim for payment of a reference lab service, where there has
been no face-to-face encounter with the beneficiary. The claim will then follow the normal
NHIC, Corp. 14 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
claims process. When a lab has a face-to-face encounter with a beneficiary, the lab is expected
to collect the MSP information and bill accordingly.
Insurance Primary to Medicare— Circumstances under which Medicare payment may be
secondary to other insurance include:
Group Health Plan Coverage:
— Working Aged;
— Disability (Large Group Health Plan); and
— End Stage Renal Disease.
No-Fault and/or Other Liability; and
Work Related Illness/Injury:
— Workers' Compensation;
— Black Lung; and
— Veterans Benefits.
NOTE: For a paper claim to be considered for Medicare Secondary Payer benefits, a copy of
the primary payer's explanation of benefits (EOB) notice must be forwarded along with the
claim form. (See Pub. 100-05, Medicare Secondary Payer Manual, Chapter 3).
CONTRACTOR NOTE: See the Medicare Secondary Payer Billing Guide in the Publications section of our website: http://www.medicarenhic.com
|
Item 11a: |
Enter the insured's 8-digit birth date (MM/DD/CCYY) and sex if different from item 3. |
|
|
Item 11b: |
Enter employer's name, if applicable. If there is a change in the insured's insurance status, |
|
|
Item 11c: |
Enter the 9-digit PAYERID number of the primary insurer. If no PAYERID numbers exist, |
|
|
Item 11d: |
Leave blank. Not required by Medicare. |
|
|
Item 12: |
|
The patient or authorized representative must sign and enter either a 6-digit date |
NHIC, Corp. 15 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
event, the statement's signature line must indicate the patient's name followed by “ by” the
representative's name, address, relationship to the patient, and the reason the patient can
not sign. The authorization is effective indefinitely unless the patient or the patient's
representative revokes this arrangement.
Note: This can be “Signature on File” and/or a computer generated signature.
The patient's signature authorizes release of medical information necessary to process the
claim. It also authorizes payment of benefits to the provider of service or supplier when the
provider of service or supplier accepts assignment on the claim.
Signature by Mark (X). When an illiterate or physically handicapped enrollee signs by
mark, a witness must enter his/her name and address next to the mark.
|
Item 13: |
|
The patient's signature or the statement “signature on file” in this item authorizes payment |
The presence of or lack of a signature or “signature on file” in this field will be indicated as such to any downstream Coordination of Benefits trading partners (supplemental insurer) with whom CMS has a payer-to-payer coordination of benefits relationship. Medicare has no control over how supplemental claims are processed, so it is important that providers accurately address this field as it may affect supplemental payments to providers and/or their patients.
In addition, the signature in this item authorizes payment of mandated Medigap benefits to the participating physician or supplier if required Medigap information is included in item 9 and its subdivisions. The patient or his/her authorized representative signs this item or the signature must be on file as a separate Medigap authorization. The Medigap assignment on file in the participating provider of service/supplier's office must be insurer specific. It may state that the authorization applies to all occasions of service until it is revoked.
NOTE: This can be “Signature on File” signature and/or a computer generated signature.
CONTRACTOR NOTE: The presence of a signature, or the statement “signature on file and/or SOF is recognized.
|
Item 14: |
|
Enter either a 6-digit (MM/DD/YY) or 8-digit (MM/DD/CCYY) date of current illness, |
NHIC, Corp. 16 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
|
Item 15: |
|
Leave blank. Not required by Medicare. |
|
Item 16: |
|
If the patient is employed and is unable to work in current occupation, enter a 6-digit |
|
Item 17: |
|
Enter the name of the referring or ordering physician if the service or item was ordered or |
The term "physician" when used within the meaning of §1861(r) of the Act and used in connection with performing any function or action refers to:
1. A doctor of medicine or osteopathy legally authorized to practice medicine and surgery by the State in which he/she performs such function or action;
2. A doctor of dental surgery or dental medicine who is legally authorized to practice dentistry by the State in which he/she performs such functions and who is acting within the scope of his/her license when performing such functions;
3. A doctor of podiatric medicine for purposes of §§(k), (m), (p) (1), and (s) and §§1814(a), 1832(a) (2) (F) (ii), and 1835 of the Act, but only with respect to functions which he/she is legally authorized to perform as such by the State in which he/she performs them;
4. A doctor of optometry, but only with respect to the provision of items or services described in §1861(s) of the Act which he/she is legally authorized to perform as a doctor of optometry by the State in which he/she performs them; or
5. A chiropractor who is licensed as such by a State (or in a State which does not license chiropractors as such), and is legally authorized to perform the services of a chiropractor in the jurisdiction in which he/she performs such services, and who meets uniform minimum standards specified by the Secretary, but only for purposes of §§1861(s) (1) and 1861(s) (2)(A) of the Act, and only with respect to treatment by means of manual manipulation of the spine (to correct a subluxation). For the purposes of §1862(a) (4) of the Act and subject to the limitations and conditions provided above, chiropractor includes a doctor of one of the arts specified in the statute and legally authorized to practice such art in the country in which the inpatient hospital services (referred to in §1862(a) (4) of the Act) are furnished.
Referring physician is a physician who requests an item or service for the beneficiary for
which payment may be made under the Medicare program.
NHIC, Corp. 17 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
Ordering physician is a physician or, when appropriate, a non-physician practitioner, who
orders non-physician services for the patient. See Pub. 100-02, Chapter 15 for non-physician
practitioner rules. Examples of services that might be ordered include diagnostic laboratory
tests, clinical laboratory tests, pharmaceutical services, durable medical equipment, and
services incident to that physician's or non-physician practitioner's service.
The ordering/referring requirement became effective January 1, 1992, and is required by §1833(q) of the Act. All claims for Medicare covered services and items that are the result of physician's order or referral shall include the ordering/referring physician's name. See Items 17a and 17b below for further guidance on reporting the referring/ordering provider's UPIN and/or NPI. The following services/situations require the submission of the referring/ordering provider information:
fl Medicare covered services and items that are the result of a physician's order
or referral;
fl Parenteral and enteral nutrition;
fl Immunosuppressive drug claims;
fl Hepatitis B claims;
fl Diagnostic laboratory services;
fl Diagnostic radiology services;
fl Portable x-ray services;
fl Consultative services;
fl Durable medical equipment
fl When the ordering physician is also the performing physician (as often is the case
with in-office clinical laboratory tests);
fl When a service is incident to the service of a physician or non-physician practitioner,
the name of the physician or non-physician practitioner who performs the initial service and orders the non-physician service must appear in item 17;
fl When a physician extender or other limited licensed practitioner refers a patient for
consultative service, submit the name of the physician who is supervising the limited licensed practitioner;
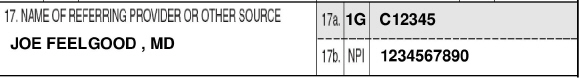
Illustration for Item 17 though 17b.
Item 17a: Enter the ID qualifier 1G, followed by the CMS assigned UPIN of the referring/ordering physician listed in item 17. All physicians who order services or refer Medicare beneficiaries must report this data.
NOTE: Effective May 23, 2008, 17a is not to be reported but 17b MUST be reported when a service was ordered or referred by a physician.
NHIC, Corp. 18 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
|
Item 17b: |
Enter the NPI of the referring/ordering physician listed in item 17. All physicians who order NOTE: Effective May 23, 2008, 17a is not to be reported but 17b MUST be reported when a CONTRACTOR NOTE: Surrogate UPINs: If the ordering/referring physician has not been The surrogate UPIN used depends on the circumstances and is used only until the physician PHS000-Physicians serving in the Public Health Serves, including the Indian Health Service Effective for services rendered January 3, 2006, and later Medicare will no longer accept the |
|
|
Item 18: |
|
Enter either an 8-digit (MM/DD/CCYY) or a 6-digit (MM/DD/CCYY) date when a |
|
Item 19: © |
Enter either a 6-digit (MM/DD/YY) or an 8-digit (MM/DD/CCYY) date patient was last seen and the UPIN (NPI when it becomes required) of his/her attending physician when a For physical therapy, occupational therapy or speech-language pathology services, effective NOTE: Effective May 23, 2008, all identifiers on the Form CMS-1500 MUST be in the form of Enter either a 6-digit (MM/DD/YY) or an 8-digit (MM/DD/CCYY) x-ray date for |
|
NHIC, Corp. 19 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
chiropractor services (if an x-ray, rather than a physical examination was the method used
to demonstrate the subluxation). By entering an x-ray date and the initiation date for course
of chiropractic treatment in item 14, the chiropractor is certifying that all the relevant information requirements (including level of subluxation) of the Pub. 100-02 Medicare Benefits Policy Manual, Chapter 15, are on file, along with the appropriate x-ray and all are available for carrier review.
Enter the drug's name and dosage when submitting a claim for Not Otherwise Classified
(NOC) drugs.
CONTRACTOR NOTE: Include route of administration if various routes are available for
administration.
Enter a concise description of an “unlisted procedure code” or an NOC code if one can be
given within the confines of this box. Otherwise, an attachment shall be submitted with the
claim.
Enter all applicable modifiers when modifier -99 (multiple modifiers) is entered in item 24d.
If modifier -99 is entered on multiple line items of a single claim form, all applicable modifiers
for each line item containing a -99 modifier should be listed as follows: 1=(mod), where
the number 1 represents the line item and “mod” represents all modifiers applicable to the
referenced line item.
CONTRACTOR NOTE: Contractors can now accept up to four modifiers on a line. If more than four are needed, use the instructions listed above.
Enter the statement "Homebound" when an independent laboratory renders an EKG
tracing or obtains a specimen from a homebound or institutionalized patient. (See Pub.
100-02, Medicare Benefit Policy Manual, Chapter 15, "Covered Medical and Other
Health Services," and Pub. 100-04, Medicare Claims Processing Manual, Chapter 16,
"Laboratory Services From Independent Labs, Physicians and Providers," and Pub. 100-
01, Medicare General Information, Eligibility, and Entitlement Manual, Chapter 5,
"Definitions," respectively for the definition of "homebound" and a more complete
definition of a medically necessary laboratory service to a homebound or an institutional
patient.)
Enter the statement, “Patient refuses to assign benefits” when the beneficiary absolutely refuses to assign benefits to a non participating physician/supplier who accepts assignment on the claim. In this case, payment can only be made directly to the beneficiary.
Enter the statement, “Testing for hearing aid” when billing services involving the testing of
a hearing aid(s) to obtain intentional denial when other payers are involved.
When dental examinations are billed, enter the specific surgery for which the exam is being
performed.
NHIC, Corp. 20 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
Enter the specific name and dosage amount when low osmolar contrast material is billed,
but only if HCPCS codes do not cover them.
Enter a 6-digit (MM/DD/YY) or an 8-digit (MM/DD/CCYY) assumed and/or relinquished date for a global surgery claim when providers share post-operative care.
Enter demonstration ID number "30" for all national emphysema treatment trial claims.
Enter theNPI/PIN of the physician who is performing a purchased interpretation of a diagnostic test. (See Pub. 100-04, Chapter 1, Section 30.2.9.1 for additional information.)
NOTE: Effective May 23, 2008, all identifiers submitted on the Form CMS-1500 MUST be
in the form of an NPI.
Method II suppliers shall enter the most current HCT value for the injection of Aranesp
for ESRD beneficiaries on dialysis. (See Pub. 100-04, Chapter 8, Section 60.7.2.)
Effective January 1, 2008, individuals and entities who bill for administration of ESAs or Part B anti-anemia drugs not self-administered (other than ESAs) in the treatment of cancer must enter the most current hemoglobin or hematocrit or hemoglobin test results. The test results shall be entered as follows: TR= test results (backslash), R1=hemoglobin, or R2=hematocrit (backslash), and the most current numeric test result figure up to 3 numerics and a decimal point[xx.x]). Examples for hemoglobin test: TR/RI9.0. Example of Hematocrit tests: TR/R2/27.0
For more information including modifiers that may apply, please see MLN Matter Article on the CMS website at
http://www.cms.hhs.gov/MLNMattersArticles/downloads/MM5699.pdf
Effective April 1, 2008, the 8-digit Clinical Trial Number may be voluntarily entered. Preface the numeric 8-digit clinical trial registry number with CT. For example, CT12345678.
CONTRACTOR NOTE: Additional conditions have been added for specific covered items. For Ambulance claims, please refer to the Ambulance Billing Guide.
|
Item 20: |
|
Complete this item when billing for diagnostic tests subject to purchase price limitations. |
NHIC, Corp. 21 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
appropriate line level information is submitted when services are rendered at different facility service locations.
NOTE: This is a required field when billing for diagnostic tests subject to purchase price
limitations.
CONTRACTOR NOTE: Only services with technical components paid under the Medicare
Physician Fee Schedule are subject to purchased diagnostic rules. Clinical laboratories are not
subject to the purchased diagnostic rules.
|
Item 21: |
|
Enter the patient's diagnosis/condition. With the exception of claims submitted by 466 19 464 00 465 0 034 0
|
|
Item 22: |
|
Leave blank. Not required by Medicare. |
|
Item 23: |
|
Enter the Quality Improvement Organization (QIO) prior authorization number for those |
Enter the Investigational Device Exemption (IDE) number when an investigational device is
used in an FDA-approved clinical trial. Post Market Approval (PMA) number should also
be placed here when applicable.
CONTRACTOR NOTE: The IDE/ PMA number has one alpha character and six numeric
digits.
For physicians performing care plan oversight services, enter the 6-digit Medicare
provider number (or NPI when effective) of the home health agency (HHA) or hospice when CPT code G0181 (HH) or G0182 (Hospice) is billed.
CONTRACTOR NOTE: Effective October 2, 1006, the requirement to include the Home Health Agency (HHA) or hospice provider number on a CPO claim is temporarily
waived by CMS. There is currently no place on the HIPAA standard ASC X 12N 837
NHIC, Corp. 22 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
format to specifically include the HHA or hospice number. Submitted claims that
include the HHA or hospice provider number will re returned to the provider as
unprocessable, until further notice
Enter the 10-digit Clinical Laboratory Improvement Act (CLIA) certification number for
laboratory services billed by an entity performing CLIA covered procedures.
CONTRACTOR NOTE: For ambulance claims, enter the zip code for the point of pick up in this field. More than one ambulance service may be reported on the same claim for a beneficiary if all points of pickup have the same ZIP code. Suppliers must prepare a separate claim for each trip if the points of pickup are located in different ZIP codes. Claims without a ZIP code in item 23, or with multiple ZIP codes in item 23, will be returned as unprocessable.
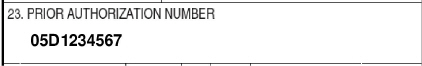
llustration for item 23.
|
|
NOTE : Item 23 can contain only 1 condition. Any additional conditions must be reported on |
|
Item 24: |
The six service lines in section 24 have been divided horizontally to accommodate When required to submit NDC drug and quantity information for Medicaid rebates, CONTRACTOR NOTE: NDC Coding may be submitted after April 7, 2008. For more |
|
Item 24A: |
Enter a 6-digit (MM/DD/YY) or 8-digit (MM/DD/CCYY) date for each procedure, |
NHIC, Corp. 23 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
|
Item 24B: |
Enter the appropriate place of service code(s) from the list provided in Section 10.5. NOTE: When a service is rendered to a hospital inpatient, use the “inpatient hospital” CONTACTOR NOTE: The Place of Service codes can be found in Appendix B of this Guide. |
|
Item 24C: |
Medicare providers are not required to complete this item. |
|
Item 24D: |
Enter the procedures, services, or supplies using the CMS Healthcare Common Procedure |
|
|
Enter the specific procedure code without a narrative description. However, when The contractor will return as unprocessable if an “unlisted procedure code” or an (NOC) CONTRACTOR NOTE: The Centers for Medicare & Medicaid Services Healthcare Common |
|
Item 24E: |
Enter the diagnosis code reference number as shown in item 21 to relate the date of service |
NHIC, Corp. 24 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
If a situation arises where two or more diagnoses are required for a procedure code (e.g., pap smears), the provider shall reference only one of the diagnoses in item 21.
04 01 2007 04 01 2007 11 99212 1
04 02 2007 04 02 2007 11 99212 2
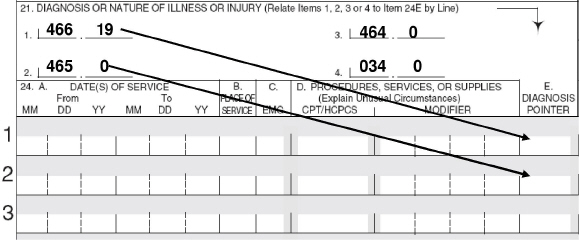
Illustration for Item 24E.
|
Item 24F: |
Enter the charge for each listed service.
Illustration for Item 24F through 24J |
|
Item 24G: |
Enter the number of days or units. This field is most commonly used for multiple visits, Some services require that the actual number or quantity billed be clearly indicated on the |
NHIC, Corp. 25 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
For anesthesia, show the elapsed time (minutes) in item 24G. Convert hours into minutes and enter the total minutes required for this procedure.
For instruction on submitting units for oxygen claims, see Pub.100-04, Chapter 20, Section
130.6
NOTE: This field should contain at least 1 day of unit. The carrier should program their system to automatically default to “1” unit when information in this field is missing to avoid returning as unprocessable.
|
Item 24H: |
Leave blank. Not required by Medicare. |
|
|
Item 24I: |
Enter the ID qualifier 1C in the shaded portion. |
|
|
Item 24J: |
Enter the rendering provider's PIN in the shaded portion. In the case of a service provided Enter the rendering provider's NPI number in the lower unshaded portion. NOTE: Effective May 23, 2008, the shaded portion of 24J is not to be reported. |
|
|
Item 25: |
|
Enter the provider of service or supplier Federal Tax I.D. (Employer Tax Identification |
|
Item 26: |
|
Enter the patient's account number assigned by the provider's of service or supplier's ac- |
|
Item 27: |
|
Check the appropriate block to indicate whether the provider of service or supplier accepts |
The following providers of service/suppliers and claims can only be paid on assignment
basis:
NHIC, Corp. 26 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
Clinical diagnostic laboratory services;
Physician services to individuals dually entitled to Medicare and Medicaid;
Participating physician/supplier services;
Services of physician assistants, nurse practitioners, clinical nurse specialists, nurse mid
wives, certified registered nurse anesthetists, clinical psychologists, and clinical social workers;
Ambulatory surgical center services for covered ASC procedures;
Home dialysis supplies and equipment paid under Method II;
Ambulance services;
Drugs and biologicals and
Simplified billing roster for influenza virus vaccine and pneumococcal vaccine
|
Item 28: |
|
Enter total charges for the services (i.e., total of all charges in item 24f). |
|
Item 29: |
|
Enter the total amount the patient paid on the covered services only. |
CONTRACTOR NOTE: We recommend this be left blank, as it is often misunderstood and can
cause incorrect payments.
|
Item 30: |
|
Leave blank. Not required by Medicare. |
|
Item 31: ® |
|
Enter the signature of the provider of service or supplier, or his/her representative, and either |
In the case of a service that is provided incident to the service of a physician or non-physician practitioner, when the ordering physician or non-physician practitioner is directly supervising the service as in 42 CFR 410.32, the signature of the ordering physician or non-physician practitioner shall be entered in item 31. When the ordering physician or non-physician practitioner is not supervising the service, then enter the signature of the physician or non- physician practitioner providing the direct supervision in item 31.
NOTE: This is a required field; however, the claim can be processed if the following is true. If a physician, supplier, or authorized person's signature is missing, but the signature is on file; or if any authorization is attached to the claim or if the signature field has "Signature on File" and/or a computer generated signature.
Item 32: Enter the name and address and ZIP code of the service location of all services other than those furnished in place of service home-12.
NHIC, Corp. 27 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
MEDICARE, MEDICARE & MORE INC
1234 HEALTHCARE STREET
ANYTOWN, CA 91234 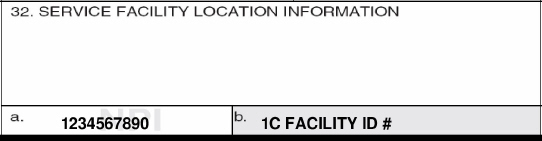
Illustration for Item 32 through 32b.
Effective for claims received on or after April 1, 2004, enter the name, address, and zip code of the service location for all services other than those furnished in place of service home –
Effective for claims received on or after April 1, 2004, on the Form CMS-1500, only one name, address and ZIP code may be entered in the block. If additional entries are needed, separate claim forms shall be submitted.
Providers of service (namely physicians) shall identify the supplier's name, address, and ZIP code when billing for purchased diagnostic tests. When more than one supplier is used, a separate Form CMS-1500 should be used to bill for each supplier.
For foreign claims, only the enrollee can file for Part B benefits rendered outside of the United States. These claims will not include a valid ZIP code. When a claim is received for these services on a beneficiary submitted Form CMS-1490S, before the claim is entered in the system, it should be determined if it is a foreign claim. If it is a foreign claim, follow instructions in Chapter 1 of IOM Publication 100-04, for disposition of the claim. The carrier processing the foreign claim will have to make necessary accommodations to verify that the claim is not returned as unprocessable due to the lack of a ZIP code.
For durable medical, orthotic, and prosthetic claims, the name and address of the location where the order was accepted must be entered (DMERC only). This field is required. When more than one supplier is used, a separate Form CMS-1500 should be used to bill for each supplier. This item is completed whether the supplier's personnel performs the work at the physician's office or at another location.
If a modifier is billed, indicating the service was rendered in a Health Professional Shortage Area (HPSA) or Physician Scarcity Area (PSA), the physical location where the service was rendered shall be entered if other than home.
If the supplier is a certified mammography screening center, enter the 6-digit FDA approved certification number.
NHIC, Corp. 28 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
Complete this item for all laboratory work performed outside a physician's office. If an independent laboratory is billing, enter the place where the test was performed.
Item 32a : If required by Medicare claims processing policy, enter the National Provider Identifier (NPI)
of the service facility.
CONTRACTOR NOTE: At the present time, only claims for purchased diagnostic services require the entry of an NPI number .
|
Item 32b: |
If required by Medicare claims processing policy, enter the PINof the service facility. Be sure NOTE: Effective May 23, 2008, Item 32b is not to be reported. |
|
|
Item 33: |
|
Enter the provider of service/supplier's billing name, address, ZIP code, and telephone |
111 555-1212
MEDICARE, MEDICARE & MORE INC.
1234 HEALTHCARE STREET
ANYTOWN, CA 91234 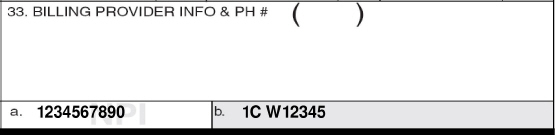
Illustration for Item 33 though 33b.
|
Item 33a : |
Enter the NPI of the billing provider or group. |
|
Item 33b: |
Enter the ID qualifier 1C followed by one blank space and then the PIN of the billing NOTE: Effective May 23, 2008, Item 33b is not to be reported. |
NHIC, Corp. 29 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
APPENDIX A – SAMPLE WORDING FOR AUTHORIZATIONS
ONE-TIME AUTHORIZATION
For Use by Provider
Beneficiary Name____________________________HIC#___________________________
I request that payment of authorized Medicare benefits be made to me or on my behalf to (Provider Name) for any services furnished me. I authorize holder of medical information about me to release to the Centers for Medicare & Medicaid Services (CMS) and its agents any information needed to determine these benefits or the benefits payable for related services.
___________________________________________Date_________________
(Beneficiary signature)
For Use by a Facility
Beneficiary Name_______________________________________HIC#________________
I request that payment of authorized Medicare benefits be made either to me or on my behalf for any services furnished me by or in (Name of Facility), including provider services. I authorize any holder of medical or other information about me to release to the Centers for Medicare & Medicaid Services (CMS) and its agents any information needed to determine these benefits or benefits for related services.
____________________________________________Date________________
(Beneficiary signature)
MEDIGAP AUTHORIZATION
Beneficiary Name________________________________________HIC#_______________
Medigap Policy Number_______________________________________
I request that payment of authorized Medigap benefits be made to either me or on my behalf to (Provider Name), for any services furnished to me by this provider. I authorize any holder of medical information to release to (Name of Medigap Insurer) any information needed to determine these benefits or the benefits payable for related services.
_____________________________________________Date_______________
(Beneficiary signature)
NHIC, Corp. 30 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
APPENDIX B - PLACE OF SERVICE CODES WITH DEFINITIONS
|
Place of |
Place of Service Name |
Place of Service Description |
|
01 |
Pharmacy |
A facility or location where drugs and other medically related items |
|
02 |
Unassigned |
N/A |
|
03 |
School |
A facility whose primary purpose is education. |
|
04 |
Homeless Shelter |
A facility or location whose primary purpose is to provide |
|
05 |
Indian Health Service |
A facility or location, owned and operated by the Indian Health |
|
06 |
Indian Health Service |
A facility or location, owned and operated by the Indian Health |
|
07 |
Tribal 638 |
A facility or location owned and operated by a federally recognized |
|
08 |
Tribal 638 Provider- |
A facility or location owned and operated by a federally recognized |
|
09 |
Prison-Correctional |
A prison, jail, reformatory, work farm, detention center, or any |
|
10 |
Unassigned |
N/A |
NHIC, Corp. 31 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
|
11 |
Office |
Location, other than a hospital, skilled nursing facility (SNF), |
|
12 |
Home |
Location, other than a hospital or other facility, where the patient |
|
13 |
Assisted Living Facility |
Congregate residential facility with self-contained living units |
|
14 |
Group Home |
A residence, with shared living areas, where clients receive |
|
15 |
Mobile Unit |
A facility/unit that moves from place-to-place equipped to provide |
|
16 |
Temporary Lodging |
Effective April 1, 2008 |
|
17-19 |
Unassigned |
N/A |
|
20 |
Urgent Care Facility |
Location, distinct from a hospital emergency room, an office, or a |
|
21 |
Inpatient Hospital |
A facility, other than psychiatric, which primarily provides |
|
22 |
Outpatient Hospital |
A portion of a hospital which provides diagnostic, therapeutic (both |
|
23 |
Emergency Room – |
A portion of a hospital where emergency diagnosis and treatment |
NHIC, Corp. 32 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
|
24 |
Ambulatory Surgical |
A freestanding facility, other than a physician's office, where |
|
25 |
Birthing Center |
A facility, other than a hospital's maternity facilities or a physician's |
|
26 |
Military Treatment |
A medical facility operated by one or more of the Uniformed |
|
27-30 |
Unassigned |
N/A |
|
31 |
Skilled Nursing Facility |
A facility which primarily provides inpatient skilled nursing care |
|
32 |
Nursing Facility |
A facility which primarily provides to residents skilled nursing care |
|
33 |
Custodial Care Facility |
A facility which provides room, board and other personal |
|
34 |
Hospice |
A facility, other than a patient's home, in which palliative and |
|
35-40 |
Unassigned |
N/A |
|
41 |
Ambulance - Land |
A land vehicle specifically designed, equipped and staffed for |
|
42 |
Ambulance – Air or |
An air or water vehicle specifically designed, equipped and staffed |
|
43-48 |
Unassigned |
N/A |
|
49 |
Independent Clinic |
A location, not part of a hospital and not described by any other |
NHIC, Corp. 33 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
|
50 |
Federally Qualified |
A facility located in a medically underserved area that provides |
|
51 |
Inpatient Psychiatric |
A facility that provides inpatient psychiatric services for the |
|
52 |
Psychiatric Facility- |
A facility for the diagnosis and treatment of mental illness that |
|
53 |
Community Mental |
A facility that provides the following services: outpatient services, |
|
54 |
Intermediate Care |
A facility which primarily provides health-related care and services |
|
55 |
Residential Substance |
A facility which provides treatment for substance (alcohol and |
|
56 |
Psychiatric Residential |
A facility or distinct part of a facility for psychiatric care which |
|
57 |
Non-residential |
A location which provides treatment for substance (alcohol and |
NHIC, Corp. 34 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
|
58-59 |
Unassigned |
N/A |
|
60 |
Mass Immunization |
A location where providers administer pneumococcal pneumonia |
|
61 |
Comprehensive Inpatient |
A facility that provides comprehensive rehabilitation services under |
|
62 |
Comprehensive |
A facility that provides comprehensive rehabilitation services under |
|
63-64 |
Unassigned |
N/A |
|
65 |
End-Stage Renal Disease |
A facility other than a hospital, which provides dialysis treatment, |
|
66-70 |
Unassigned |
N/A |
|
71 |
Public Health Clinic |
A facility maintained by either State or local health departments |
|
72 |
Rural Health Clinic |
A certified facility which is located in a rural medically |
|
73-80 |
Unassigned |
N/A |
|
81 |
Independent Laboratory |
A laboratory certified to perform diagnostic and/or clinical tests |
|
82-98 |
Unassigned |
N/A |
|
99 |
Other Place of Service |
Other place of service not identified above. |
NHIC, Corp. 35 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
NHIC, Corp. 36 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
TELEPHONE AND ADDRESS DIRECTORY
Provider Interactive Voice Response (IVR) Directory
All actively enrolled providers must utilize the IVR for: Beneficiary Eligibility, Deductible, Claim Status, Check Status and Earnings to Date. The IVR can also assist you with the following
information: Seminars, Telephone Numbers, Addresses, Medicare News and Appeal Rights.
|
Available 24 hours/day, 7 days/week (including holidays) 1-877-591-1587 |
|
California Northern |
|
Available 24 hours/day, 7 days/week (including holidays) 1-877-591-1587 |
Provider Customer Service Directory
Our Customer Service representatives will assist you with questions that cannot be answered by the IVR, such as policy questions, specific claim denial questions, 855 application status, redetermination status (formerly Appeals). Per CMS requirements, the Customer Service representatives may not assist providers with Beneficiary Eligibility, Deductible, Claim Status, Check Status and Earnings to Date unless we are experiencing IVR system problems. This rule applies even if the caller has obtained the code.
Hours of Operation: 8:00 a.m. to 4:00 p.m. Monday – Friday
|
California |
1-877-527-6613 |
|
New England Maine |
1-877-258-4442 |
NHIC, Corp. 37 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
MAILING ADDRESS DIRECTORY
|
Northern California Medicare Provider Certification |
P.O. Box 2812 |
|
|
Medicare Preferred Provider |
P.O. Box 2804 |
|
|
Medicare Secondary Payer |
|
P.O. Box 2004 |
|
MSP Cash |
Marysville, CA 95901-951 |
|
|
Medicare Written Inquiries/MSP |
P.O. Box 2006 |
|
|
Medicare Redetermination |
P.O. Box 2800 |
|
|
Medicare Payment Safeguard |
P.O. Box 2806 |
|
|
Medicare EDI |
P.O. Box 2807 |
|
Medicare ADS (Automated Development System) P.O. Box 2009
Chico, CA 95927-2009
|
Medicare Redetermination O/P |
P.O. Box 2808 |
|
Cash Accounting |
P.O. Box 391 |
|
Medicare Reconsideration |
P.O. Box 2811 |
NHIC, Corp. 38 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
|
Southern California Medicare Claims |
P.O. Box 272852 |
|||
|
Medicare Secondary Payer |
P.O. Box 272855 |
|||
|
Overpayment Recoup Checks |
P.O. Box 515301 |
|||
|
Medicare Overpayments (Undeliverable Checks) |
P.O. Box 515302 |
|||
|
Medicare Written Inquiry |
P.O. Box 272857 |
|||
|
Medicare Redetermination |
P.O. Box 272854 |
|||
|
Medicare Administrative Mail |
P.O. Box 54905 |
|||
|
California - Benefit Integrity Support (BISC) |
P.O. Box 51447 |
|||
|
Medicare Electronic Data Interchange (EDI) |
P.O. Box 2807 |
|||
|
Medicare ADS |
P.O. Box 272859 |
|||
|
Undeliverable Mail |
|
P.O. Box 54113 |
||
|
Third Party Liability (TPL)/ |
P.O. Box 515391 |
|||
|
Medicare Redetermination Overpayment |
|
P.O. Box 2808 |
||
|
Medicare Reconsideration |
|
P.O. Box 515300 |
||
NHIC, Corp. 39 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
New England
|
Initial Claim Submission Maine |
P.O. Box 2323 |
|
|
Massachusetts |
P.O. Box 1212 |
|
|
New Hampshire |
P.O. Box 1717 |
|
|
Vermont |
P. O. Box 7777 |
|
|
EDI (Electronic Data Interchange) |
|
P.O. Box 9104 |
|
Written Correspondence/Overpayments/ |
P.O. Box 1000 |
|
|
Medicare B Refunds |
Medicare B Accounting Control |
|
|
Medicare Secondary Payer |
P.O. Box 9100 |
|
|
Provider Enrollment |
P.O. Box 3434 |
|
|
Program Safeguard Contractor (PSC) |
P.O. Box 4444 |
|
NHIC, Corp. 40 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
Durable Medical Equipment (DME)
For information, please contact the DME Regional Contractor for your area.
California Durable Medical Equipment (DME) Contractor:
Noridian Administrative Services General Medicare Information: 1-866-243-7272
Please view the website to find the appropriate address:
https://www.noridianmedicare.com/dme/contact/contact.html
New England Durable Medical Equipment (DME) Medicare Administrative Contractor:
NHIC, Corp. Provider Service Line: 1-866-419-9458
Please view the website to find the appropriate address:
http://www.medicarenhic.com/dme/contacts.shtml
Reconsideration (Second Level of Appeal)
New England and California
First Coast Service Options Inc.
QIC Part B North Reconsiderations
P.O. Box 45208
Jacksonville, FL 32232-5208
NHIC, Corp. 41 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
INTERNET RESOURCES
The Internet is a very valuable tool in researching certain questions or issues. NHIC has a comprehensive website that serves as a direct source to Medicare as well as a referral tool to other related websites that may prove to be beneficial to you.
NHIC, Corp.
http://www.medicarenhic.com
Upon entering NHIC's web address you will be first taken straight to the “home page” where there is a menu of information. NHIC's web page is designed to be user-friendly.
We encourage all providers to join our website mailing list. Just click the link on the home page entitled “Join Our Mailing List”. You may also access the link directly at: http://visitor.constantcontact.com/email.jsp?m=1101180493704
When you select the “General Website Updates”, you will receive a news report every week, via e-mail, letting you know what the latest updates are for the Medicare program. Other Web News selections (CA Updates, NE Updates, EDI, etc.) will be sent out on an as-needed basis.
Provider Page Menus/Links
From the home page, click either the “California Providers” or “New England Providers” link. This will take you to the License for use of "Physicians' Current Procedural Terminology", (CPT) and "Current Dental Terminology", (CDT). Scroll down to bottom of the page. Once you click “Agree”, you will be taken to the provider pages.
On the left side of the web page you will see a menu of topics that are available. Explore each one and bookmark those that you use most often.
Medicare Coverage Database
http://www.cms.hhs.gov/center/coverage.asp
http://www.cms.hhs.gov/mcd/indexes.asp
The Medicare Coverage Database is an administrative and educational tool to assist providers, physicians and suppliers in submitting correct claims for payment. It features Local Coverage Determinations (LCDs) developed by Medicare Contractors and National Coverage Determinations (NCDs) developed by CMS. CMS requires that local policies be consistent with national guidance (although they can be more detailed or specific), developed with scientific evidence and clinical practice.
Medicare Learning Network
http://www.cms.hhs.gov/MLNGenInfo/
The Medicare Learning Network (MLN) website was established by CMS in response to the increased usage of the Internet as a learning resource by Medicare health care professionals. This website is designed
NHIC, Corp. 42 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
to provide you with the appropriate information and tools to aid health care professionals about Medicare. For courses and information, visit the web site. For a list of the Training Programs, Medicare Learning Network Matters articles and other education tools available, visit the website.
Open Door Forums
http://www.cms.hhs.gov/OpenDoorForums/
CMS conducts Open Door Forums. The Open Door Forum addresses the concerns and issues of providers. Providers may participate by conference call and have the opportunity to express concerns and ask questions. For more information, including signing up for the Open Door Forum mailing list, visit the website.
Publications and Forms
http://www.cms.hhs.gov/CMSForms/
http://www.cms.hhs.gov/MedicareProviderSupEnroll/
For your convenience CMS has published optional forms, standard forms, and SSA forms. By linking onto the Publications site you can access the following forms:
For your convenience CMS has published optional forms, standard forms, and SSA forms. By linking onto this website, you can access numerous CMS forms such as:
Provider Enrollment CMS 855 forms (CMS 855B, 855I, & 855R)
Medicare Participating Physician or Supplier Agreement (CMS 460)
Advanced Beneficiary Notices (ABN) (CMS R-131- G, R-131-L, & 20007)
Medicare Redetermination Request Form (CMS 20027)
Request for Hearing (CMS 1965)
Medicare Managed Care Disenrollment form (CMS 566)
|
Advance Beneficiary Notice (ABN) |
http://cms.hhs.gov/BNI/ |
|
American Medical Association |
http://www.ama-assn.org/ |
|
CMS |
http://www.cms.hhs.gov |
|
CMS Correct Coding Initiative |
http://www.cms.hhs.gov/NationalCorrectCodInitEd/ |
|
CMS Physician's Information |
http://www.cms.hhs.gov/center/physician.asp? |
|
Evaluation & Management |
http://www.cms.hhs.gov/MLNEdWebGuide/25_EMDOC.asp |
NHIC, Corp. 43 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
CMS-1500 Claim Form Instructions
________________________________________________________________________
|
Federal Register |
http://www.archives.gov/federal-register |
|
HIPAA |
http://www.cms.hhs.gov/HIPAAGenInfo/ |
|
National Provider Identifier (NPI) |
http://www.cms.hhs.gov/NationalProvIdentStand/ |
|
NPI Registry |
https://nppes.cms.hhs.gov/NPPES/NPIRegistryHome.do |
|
U.S. Government Printing Office |
http://www.gpoaccess.gov/index.html |
NHIC, Corp. 44 February 2008
REF-EDO-0003 Version 8.0
Message for internal use only: The master copy of this document is stored in the NHIC ISO Documentation Repository. Any other copy, either electronic or paper, is an uncontrolled copy and must be deleted or destroyed when it has served its purpose.
NHIC, Corp.
75 Sgt. William Terry Drive Hingham, MA 02044
1055 West 7th Street
Los Angeles, CA 90017
620 J Street
Marysville, CA 95901
Website:
http://www.medicarenhic.com
CMS Websites
http://www.cms.hhs.gov
http://www.medicare.gov
REF-EDO-0003 Version 8.0