
Intellect™
CHARGES MENU OPTIONS

Claim Scrubbing Feature Overview
Option available in Version 9.12.01
What Is Claim Scrubbing?
Claim Scrubbing is a process where, prior to billing, the clinic's diagnosis and procedure information is transmitted 'real time' to a vendor who passes the claim through a series of edits. Any errors are immediately reported in a pop up window on the clinic's claims entry screen - allowing staff to correct the claim at that time. Claim Scrubbing can dramatically decrease the percentage of rejected and denied claims.
Effective 5/1/2025, Optum clearinghouse no longer offers the Provider Advance Claim Edit (ACE) product for claim scrubbing integration with Intellect.
This document includes:
What Types of Scrubbing Edits are Applied?
How Do I Sign Up for Claim Scrubbing?
What Are The System Requirements To Use Claim Scrubbing?
Intellect Interface for Claim Scrubbing
What Types Of Scrubbing Edits Are Applied?
Optum (formerly Ingenix /ENS):
CPT Codes to DX Modifier relationships
Sequencing of DX codes
Appropriate use of Modifiers
Age, Gender, Frequency relationships
Medicare unbundle (CCI)
Medicare Edits (MUE, Globals, Reductions)
Non-covered services
Commercial unbundle edits
NCD/LCD
Missing charges
Duplicate charges
Validation edits (CPT, HCPCS, ICD-9)
Historical edits
How Do I Sign up For Claim Scrubbing, And Are There Any Costs?
Integration with Intellect is no longer available through third-party clearinghouse.
What Are The System Requirements To Use Claim Scrubbing?
Clients must be running version 09.12.01 or greater of Intellect to use Claim Scrubbing. A support agent verifies the Intellect version, and contacts the clinic to schedule an update, if needed.
The server and each workstation using the Claim Scrubbing feature must have a current jre file. The file is included in the program update, and is located in the home/staff/app/tmp folder, named jre1.6.zip. Manually unzip the file by right-clicking and selecting Extract All. Failure to do this results in the error message 'Could not find trusted certificate.'
Intellect Interface for Claim Scrubbing
There is a [Scrub] button on the Charges screen to facilitate claims scrubbing. The [Scrub] button is located in the Post Options section in the bottom right corner, as shown below:
Diagnoses and charges are posted as usual. Before committing the charge(s), the [Scrub] button is clicked. An XML file is then submitted to the vendor via sftp (secure file transfer protocol), and a message file is returned with the results. When a claim is scrubbed and charges committed, the program inserts a copy of the message into the second screen of the ledger - both Accounting and Open Item.
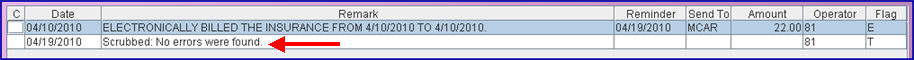
• When no errors are found, the vendor returns a response 'No errors were found,' as shown below:
Note: Prior to Version 9.12.08, the Flag for the comment was T (see below). Because Flag T is used for another purpose, the claim scrubbing Flag was changed. Effective update 9.12.08, it is now Flag V.
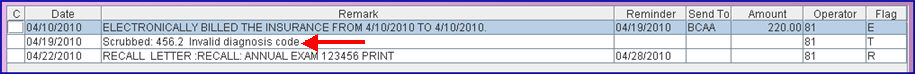
• If the scrubber finds errors, a message is returned indicating what the error is. An example is shown below.
Note: Prior to Version 9.12.08, the Flag for the comment was T (see below). Because Flag T is used for another purpose, the claim scrubbing Flag was changed. Effective update 9.12.08, it is now Flag V.
Other error messages that could be displayed might be:
o Wrong age for procedure
o Wrong age for diagnosis
o Wrong gender for procedure
o Wrong gender for diagnosis
o Invalid Modifier
o Invalid Place of Service
This feature needs to be set up before it may be used. Once the Claims Scrubbing feature has been set up, it can be used on the Charges screen located at Charges --►Charges.
Set up the system as follows:
1. Sign-up with supported third-party vendor.
2. Set up an Insurance Co. Code called CCI. This is not a real insurance company, but a CCI insurance code needs to be set up for scrubbing to work.
2.1 Go to Utility --► Insurance --► Insurance
2.2 To set up the CCI insurance code, only these two fields need to be filled:
2.2.1 <Insurance Co. Code>: Enter CCI
2.2.2 <Name>: Enter CCI - do not delete
2.3 Click on the [Add] button.
3. After the CCI insurance company code has been added, the CCI insurance needs to be set up at Utility --► Insurance --► Tele Com as follows:
For Optum (formerly Ingenix/ENS):
3.1 <Insurance Code>: Type in CCI.
3.2 <Submission Script>: This field should automatically populate.
3.3 <Login>: Enter the login as assigned by the vendor.
3.4 <Password>: Enter the login as assigned by the vendor.
3.5 <Transmission Method>: From the drop-down list, select:
• INGENIX_EDITING: To allow Optum (formerly Ingenix/ENS) to run ACE (Advanced Clinical Editing) scrubbing against the claims.
• INGENIX_ROUTING: To allow Optum (formerly Ingenix/ENS) to run ACE (Advanced Clinical Editing) scrubbing against claims and send the error-free claims to the Payers.
3.6 <FTP Site>: Select the Optum (formerly Ingenix/ENS) site as shown below:
4. Once the claims scrubbing feature has been set up, it can be used on the Charges screen located at Charges --►Charges.
Following are the claim scrubbing errors when the Utility --► Insurance --► Tele Com screen is not set up for Claim Scrubbing.

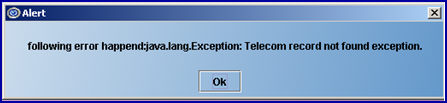
This message appears when there is a problem with the certificate:
