Intellect™
CHARGES MENU OPTIONS

Specialty Charges
Epogen Charge Set Up
A physician-administered drug includes any covered outpatient drug provided or administered to a recipient, which is billed by a provider other than a pharmacy. Such providers would include, but not be limited to, physician offices, clinics, and hospitals. A covered outpatient drug is broadly defined as a drug that may be dispensed only upon prescription and is approved for safety and effectiveness as a prescription drug under the Federal Food, Drug, and Cosmetic Act. Physician-administered drugs are not restricted to injectable drugs only. Physician-administered drugs include any drug regardless of the method of administration.
Such claims need to include NDCs, corresponding quantity amounts, Unit of Measure, and a prescription number for physician-administered drugs.
Three screens need to be set up when billing appropriate physician-administered drugs for electronic claims submission:
Utility --►Procedure --►Procedure --►Add
Charges --► Encounter--►Epogen
See also Paper Claims Reference Information.
Utility --►Procedure --►Procedure --►Add
Create a Panel Code for the particular drug. This may be a single panel or part of another panel. Complete this screen as normal with these fields included:
1. Status 
1.1 Set this field to 'N.' It is used to include the necessary NDC information when submitting the electronic claim.
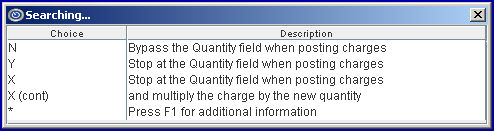
[Name change effective version 13.10.29 - formerly QTY (Y/N/X)]
2.1 This field determines whether or not the cursor stops at the Charges --► Charge <QTY> field when posting charges.
2.2 Set to 'Y' if quantities need to be adjusted at posting.
3. NDC Number 
3.1 This field is used for electronic billing of claims. If completed, the National Drug Code number is submitted in the electronic claim in Segment LIN, Loop 2410.
3.2 Enter the 11-digit NDC code without hyphens or the qualifier (Intellect adds the qualifier).
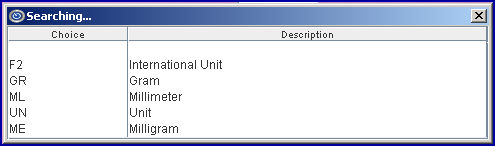
4. Unit of Measure 
4.1 The <Unit of Measure> is required when an NDC Code is present.
4.2 Select the Composite Unit of Measure Qualifier that applies to the billing in this field. It is used to populate the Electronic 837 claim Loop 2410 CTP05.
5. NDC Unit Value 
5.1 This is used to convert quantities from HCPCS to NDC.
5.2 This value populates the Electronic 837 claim Loop 2410 CTP04.
5.3 Type the actual decimal quantity administered in a single dose.
For the following example, 0.2 would be entered:
HCPCS code is per 10mg and the product comes as a dry powder injection 500mg
NDC units are 'each vial'
Dose was 100 mg
Resulting in: HCPCS quantity = 10 and the NDC quantity = 100/500 = 0.2
Charges --► Encounter --►Epogen
Create a record for each patient with a claim. Complete these fields:
6.1 This is used in electronic claims submission, Loop 2400 MEA01.
6.2 It is required on service lines which bill/report Concentration, Hemoglobin, Hematocrit, Epoetin Starting Dosage, Creatin, and Oxygen.
6.3 Indicate the type of measurement that applies to <Measurement Value 1>.
NOTE: Epoetin starting dosage, in MEA-02. OG is only valid when reported with R3. When sending test results, use the qualifier "TR". Test results should reflect a measurement qualifier, other than R3 (Epoetin starting dosage).
7.1 This is used in electronic claims submission, Loop 2400 MEA03.
7.2 Enter the value of the measurement that applies to <Measurement Qualifier 1>.
The test results should be entered as follows: TR = test results, R1=hemoglobin or R2=hematocrit (a 2-byte alpha-numeric element), and the most recent numeric test result (a 3-byte numeric element, decimal implied [xx.x]). Results exceeding 3-byte numeric elements (10.50) are reported as 10.5.
Examples: If the most recent hemoglobin test results are 10.50, providers should enter: TR/R1/10.5. Or, if the most recent hematocrit results are 32.3, providers would enter: TR/R2/32.3.
8.1 This is used in electronic claims submission in Loop 2400 MEA02. It is a code identifying a specific product or process characteristic to which a measurement applies.
8.2 This code is required on service lines for Dialysis for ESRD End-Stage Renal Disease (ESRD).
8.3 Select the appropriate code from the drop-down list:
Use R1, R2, R3, or R4 to qualify the Hemoglobin, or Hematocrit (Ht or HCT), and Epoetin Starting Dosage, and Creatinine test results. The percentage by volume of packed red blood cells in a given sample of blood after centrifugation and packed cell volume (PCV) are measures of the proportion of blood volume that is occupied by red blood cells. It is normally between 45 +/- 7 (38-52%) for males and between 42 +/- 5 (37-47%) for women.
9.1 Used in electronic claims submission, Loop 2400 DTP*739.
9.2 This is required on initial EPO claims service lines where test results are being billed/reported.
9.3 Enter the most recent Serum Creatin test date.
10.1 Used in electronic claims submission, Loop 2400 DTP*738.
10.2 This is required on initial EPO claims service lines where test results are being billed/reported.
10.3 Enter the most recent Hemoglobin or Hematocrit test date or both.
11. Rx Number 
11.1 Enter the unique identification number assigned by the pharmacy or supplier for the prescription.
11.2 This uses Loop 2410 REF02 with the Qualifier XZ automatically added by Intellect.
Post charges as normal, noting:
12. EN# 
12.1 Complete the <EN#> field with the encounter number containing the number for this patient.
Paper Claims Reference Information
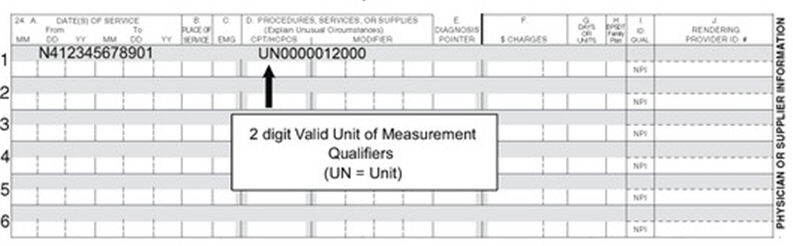
Intellect completes Box 24A CMS 1500 (HCFA) in the gray-shaded area with the NDC number proceeded by the 'N4' qualifier.

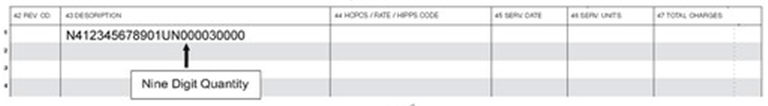
Or, on the UB-04 claim form, Intellect completes the Description field (Box 43) including the Unit of Measure and the Quantity.
Intellect completes Box 24D CMS 1500 (HCFA) in the gray-shaded area with the quantity preceded by the Unit of Measure qualifier