
Intellect™
CHARGES MENU OPTIONS

Specialty Charges
Physician Quality Reporting Initiative Set Up in Intellect
Note: 2016 was the last program year for PQRS. PQRS transitioned to the Merit-based Incentive Payment System (MIPS) under the Quality Payment Program. The final data submission timeframe for reporting 2016 PQRS quality data to avoid the 2018 PQRS downward payment adjustment was January through March 2017. The first MIPS performance period was January through December 2017. For more information, please visit the Quality Payment Program website.
Prime Clinical Systems, Inc recommends the following set up for providers enrolled in the Medicare PQRI program:
1. For reporting purposes in Intellect, we suggest offices add a new Utility --► Procedure <Category> code for their PQRI procedures. Offices may prefer to add multiple Procedure Category codes; i.e., one for each type of PQRI procedure. Adding a new code is a two-step process. Please complete these steps:
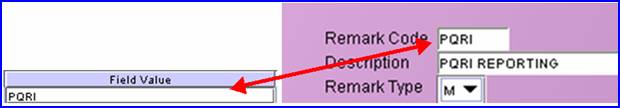
1.1 Go to Utility --►Messages --►Remark --►Add.

Complete the screen as indicated:
1.1.1 <Remark Code>: Enter the Utility --► Procedure <Category> code.
1.1.2 <Description>: Enter the description as they should appear on reports.
1.1.3 <Remark Type>: Select 'M' for Management Reports.
1.1.4 Click on the [Add] button to save the record.
1.2 Go to Utility --►Set Up --►Field Choices --►Modify:
1.2.1 At the <Field Name> field enter PR_GROUP
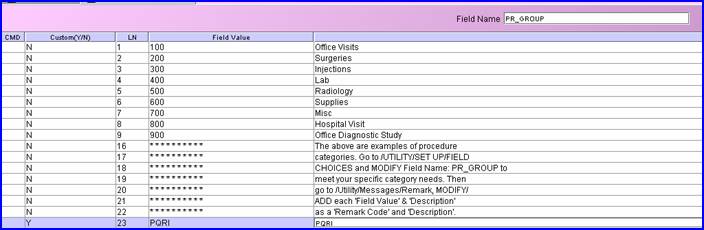
1.2.2 A list of existing Utility --► Procedure <Category> codes should display The above list is only an example, each clinics' list may be different.
1.2.3 With the focus in the <CMD> (command) column, press the letter A on the keyboard to add a new record.

1.2.4 <Custom (Y/N)>: Type 'Y' (yes) to flag the record as customized so future updates will not be able to change the record:
![]()
1.2.5 <LN>: The focus skips this column.
1.2.6 <Field Value>: Enter the new Procedure Category code. This must match the new code entered in Utility --►Messages --►Remark (see step 1.1 above).
1.2.7 <Description>: Enter the description as it should appear on reports.
1.2.8 After entering the Description, the focus returns to the <Field Value> column.
1.2.8.1 If adding only one new code, exit by pressing the [Esc] key until the program is back at the Utility --►Set Up --►Field Choices menu.
1.2.8.2 If adding more than one new code, continue with steps 1.2.5 and 1.2.6 until completed. Then press the [Esc] key until the program is back at the Utility --►Set Up --►Field Choices menu. Be as specific and add as many descriptions as desired in order for the Management reports to record the PQRI initiatives.
2. Add a new Utility --►Procedure <Panel Code> for each PQRI procedure which applies.
2.1 Complete the Procedure screen as usual EXCEPT enter .01 in the <Charge Global> field.
2.2 Select the PQRI <Category> code from the drop-down list:
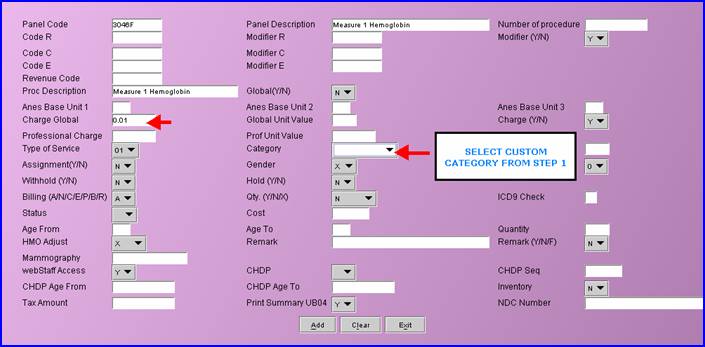
2.3 Click on the [Add] button to save the record.
Note: For a procedure to be billed electronically, it must have a charge amount greater than zero.
3. Post charges through Charges --►Charge:
Post any PQRI procedure in addition to the charges which would normally be posted to the patient's chart.
Note: The Adjustment may be posted either in the Charges --►Charge or the Payment --►Open Item screen. Prime Clinical Systems recommends the adjustment be posted through Payment --►Open Item for more accurate Management reports.
3.1 If posting in Charges --►Charge, the adjustment code pulls from the Utility --►Category <Pt Adjustment Remark>. The Adjustment Remark may not be changed while posting adjustments in the Charge screen. Prime Clinical Systems recommends offices do NOT modify the Utility --►Category <Pt Adjustment Remark> as it is used for other types of adjustments which may print on reports or patient statements.
Post an adjustment on the Charge screen of .01 cent for each PQRI procedure posted as follows:
3.1.1 In the <C> (command) column, press the letter 'M' to modify the line.
3.1.2 Press the [Enter] key until the focus is in the <Adjustment> column.
3.1.3 Type .01 then press the [Enter] key until the focus is in the <C> (command) column.
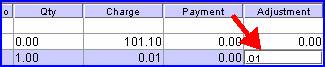
3.1.4 Repeat this process for each PQRI procedure.
3.1.5 Click on the [Commit All] button to save the charges and adjustments.
3.2 If posting in Payment --► Open Item, the Source of Adjustment code defaults from the Utility --►Insurance screen <Adjustment Source> field. This can be modified when posting in Payment --►Open Item.
For offices posting adjustments through Payment --►Open Item who wish to add PQRI Adjustment Remarks:
3.2.1 Go to Utility --►Messages --►Remark --►Add:

3.2.2 Complete the screen as indicated:
3.2.2.1 <Remark Code>: Enter a code for a PQRI Adjustment.
3.2.2.2 <Description>: Enter the description as it should appear on reports.
3.2.2.3 <Remark Type>: Select 'A' for Adjustment Remark, and click on the [Add] button to save the record.
3.2.3 Next, go to Payment --► Open Item:
![]()
3.2.4 Complete the information, changing the <Src Adjustment> field to the PQRI adjustment code set up in step 3.2.2, and verify that <Method> = I:
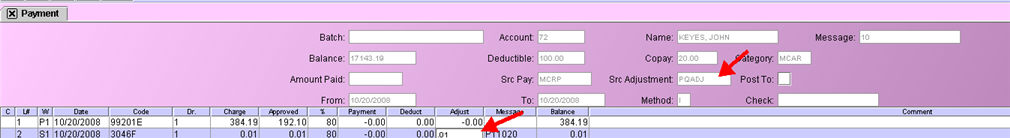
3.2.4.1 With the focus in the Command Column for the PQRI Charge, type 'M' to modify. Press [Enter] until the focus is in the <Adjust column>, type .01, and press [Enter] until the focus is back in the Command Column.
3..2.4.2 When finished with all adjustments, commit by either typing 'C' in the Command Column OR pressing the [Commit/Exit] button.
NOTE: If the Utility --► Set Up --► Parameter <Include Zero Charges> field = 'Y,' then the PQRI .01 cent procedure and .01 cent adjustment prints on the patient statement.
NOTE: The Medicare, Medicaid, and SCHIP Extension Act of 2007 (MMSEA) authorized CMS to establish alternative methods to report 2008 Physician Quality Reporting Initiative (PQRI) quality data, including the option of reporting on a group of clinically-related measures. Four Measures Groups have been established for 2008 PQRI: 1) Diabetes Mellitus, 2) End Stage Renal Disease (ESRD), 3) Chronic Kidney Disease (CKD), and 4) Preventive Care. These four groups, which combined include a total of 22 measures, may be reported through either claims-based or registry-based submission.
In order to identify the intention to report a measures group, submit a measures group-specific G-code on a claim for covered professional services furnished to a patient enrolled in Medicare Part B Fee-For-Service:
G8485: I intend to report the Diabetes measure grouping;
G8488: I intend to report the End Stage Renal Disease (ESRD) measure grouping;
G8487: I intend to report the Chronic Kidney Disease (CKD) measure grouping;
G8486: I intend to report the Preventive Care measure grouping.
For more information on the Medicare PQRI program, refer to these web sites:
PQRI Home
PQRI Reporting
PQRI FAQ