OnSTAFF 2000
Billing/Menu
This menu allows you to bill the financially responsible party by sending either an insurance form (paper or electronic) or a detailed statement.
Menu Options:
Insurance Allows billing of Insurance claim forms to the applicable insurance company.
Statement This option allows the printing of detailed statements, which are sent to patients.
Tele Com This option is used for electronic claims submission.
Follow-Up Used to generate follow-up letters to patients or insurance carriers.
Worker Used to bill charges and submit other Workers Compensation related information.
Pre-Billing Allows you to, prior to billing, for ALL charges entered, edit the information contained in the report.
Exit Returns you to the Main Menu.
Billing / Tele Com / ANSI Features
New Menu Option: ANSI Features

ANSI Features is used to request from Medicare the following electronic features:
|
ANSI 997 Report Acknowledgement / Error Summary Report Eligibility Request Eligibility Report |
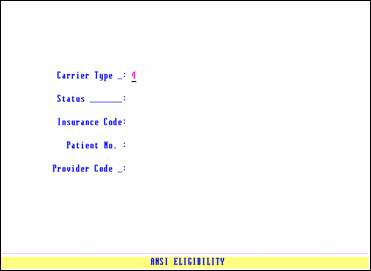
Carrier Type: 4 - Medicare
Status: Pressing the [F2] search key will display the following valid choices:
9 ANSI 997 Report (see below ‘Sample ANSI 997 Report’)
A Error Summary Report (i.e., Acknowledgement)
S IN THE FUTURE Eligibility Request (Send request)
P IN THE FUTURE Eligibility Report (Pick up report)
As of version 8.2 10/06/2011, programming is completed to accommodate ANSI 5010 requirements which are effective January 1, 2012. The current ANSI 997 Report has been replaced with the new ANSI 999 Report and reads (basically) the same. There is a new Segment(s) on the ANSI 999 Report, a line(s) beginning with 'IK'; for example, the line 'IK5*A~' indicates the claim was 'A'ccepted. If the claim was 'R'ejected, this line would read 'IK5*R~'. For any 'R' (rejections) in ANY 'IK' fields/lines of the ANSI 999 Report, fax your ANSI 999 Report to PCS at 616-449-5615. Include your client ID, contact person, and phone number. Click here for a 999 Report sample.
Also effective January 1, 2012, the new ANSI 277CA Report (Claim Acknowledgement) replaces the current Claim Acknowledgement/RSP report which is no longer available with ANSI 5010. The 277CA file will be converted to a report form and printed. Click here for a 277CA Report sample.
Insurance Code: Enter the /Utility/Insurance <Insurance Co. Code> for Medicare, press [Enter], then enter the /Utility/Insurance <Insurance Co. Code> for Medi-Medi, press [Enter].
Patient No.: When using <Carrier Type> = 4 and the following <Status> options:
9 Automatically bypasses this field.
A Automatically bypasses this field.
S Enter the account number(s) of the patient(s) whose eligibility you want verified by Medicare, then press the [é] key to continue to the next field.
P Automatically bypasses this field.
Provider Code: Optional.
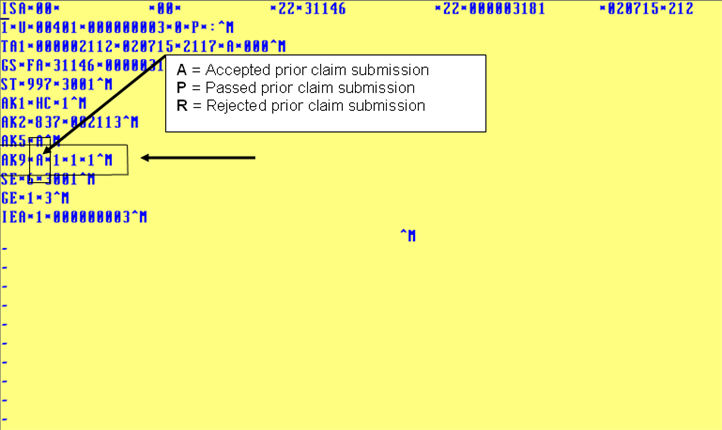
Sample ANSI 997 Report:
Note: As of January 1, 2012, this report will no longer be available. It is being replaced by the 999 Report which reads similarly to the 997 report. See the <Status> field information for a link to a 999 Report sample.
|
|
HOW TO READ THE ANSI 997 Report:
To determine Medicare’s response as to whether your claims for the prior submission were accepted or rejected, locate the line which begins with AK9. On that line, AK9 will be immediately followed by an A (accepted), P (passed), or R (rejected). The above example denotes Medicare’s acceptance of a prior electronic claim submission.
WHEN TO USE THE ANSI 997 Report:
Twenty-four hours after electronic claim submission, request the ANSI 997 Report. If the report indicates:
1. The prior submission was accepted, you may request the Acknowledgement / Error Summary Report.
2. The prior submission was rejected, fax the ANSI 997 Report to Software Support at (626) 449-5615. Include your client ID, contact person, job ID, and the date the report was printed. A reference will be opened and you will receive a call back.