Billing/Menu
This menu allows you to bill the financially responsible party by sending either an insurance form (paper or electronic) or a detailed statement.
How Medicare EDI Claims are Processed
Menu Options:
Insurance Allows billing of Insurance claim forms to the applicable insurance company.
Statement This option allows the printing of detailed statements, which are sent to patients.
Tele Com This option is used for electronic claims submission.
Follow-Up Used to generate follow-up letters to patients or insurance carriers.
Worker Used to bill charges and submit other Workers Compensation related information.
Pre-Billing Allows you to, prior to billing, for ALL charges entered, edit the information contained in the report.
Exit Returns you to the Main Menu.
Billing/Insurance/Tele Com Submit
How to use the <Primary/Sec/All(P/S/A)> and <All/Unbill/Rebill(A/U/R/H)> fields of the /Billing/Insurance screens:
|
|
|
Standard Software Requirements For All Options:
1) A charge/date of service exists within the requested date range
2) The requested insurance(s) exist as one of the patient’s insurance screen(s)
3) The date(s) of service fall within the insurance screen’s <Coverage From> and <To> date range
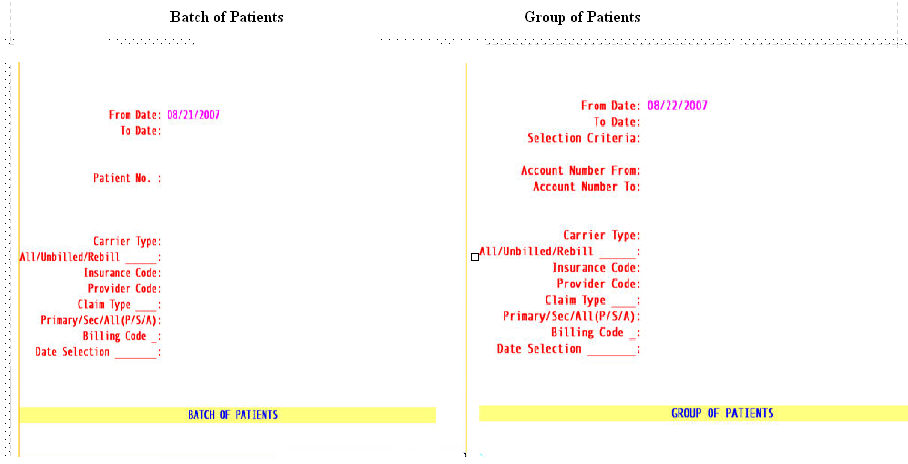
From Date
The beginning date of the date range for charges to be billed/rebilled based on the <Date Selection> field criteria.
To Date
The latest date of the date range for charges to be billed/rebilled based on the <Date Selection> field criteria.
Patient Number or Selection Criteria
For Batch type the patient account number.
The system will display a batch entry screen enabling the user to enter more accounts up to a total of 99.
For Group entry
1. Allows user to define the accounts to bill based on alphabetical criteria.
Press [Enter] to select all patients that meet any other criteria entered below or define the parameter using an alphabetical range hyphenated and bracketed such as [A-M] to return patient accounts where the last name begins with any letters in the range of A-M.
![]()
2. Account Number From :
This is the beginning number for billing by a specific range of patient account numbers. You may bypass this field by pressing [Enter] thus requesting ALL accounts or you may use this field as the beginning account number to be billed.
3. Account Number To:This is the ending number for billing by a specific range of patient account numbers. You may bypass this field by pressing [Enter] thus requesting ALL accounts greater than any value entered in < Account Number From > (open ended) or you may use a this field as the ending account number to be billed.
Note: when pressing [Enter] without entering an account number in one of the fields the following message will be displayed urging you to enter values: