
OnSTAFF 2000
CAPITATED (PRE-PAID) POSTING
Meeting the following Software requirements allows you to use the Auto Payment feature for Capitated (Pre-Paid) Contracts. Using this feature will distribute your monthly cap check over all patients seen the previous month, printing a report noting the patient, charge, payment and adjustment. In this way, you will be able to track month to month, per contract, your charges and payments thus giving you the tool to determine whether or not to continue with this contract or re-negotiate. You may also use the printed report to confirm each patient against the carriers current eligibility listing. The Software requirements must be met PRIOR TO POSTING CHARGES in order for the Auto Payment feature to function properly and will affect ONLY patient’s who have been assigned a pre-paid category type.
Software Requirements for Auto Payment Posting for Capitated (Pre-Paid) accounts:
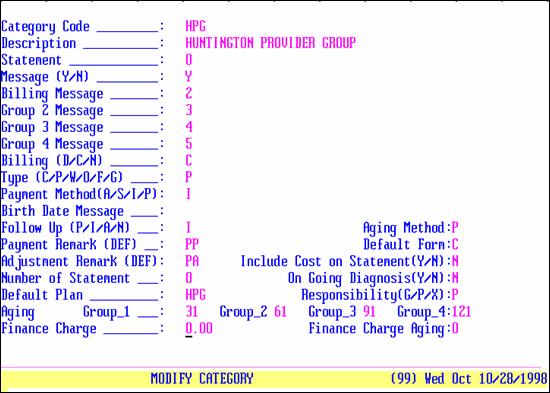
/Utility/Category:
Set up a category for each individual Capitated contract. This category will be entered on the /New Patient Category field for those patients who are part of this contract and will be used when distributing the monthly cap check. Having a category for each contract will be advantageous in follow up and management reports. Fill in each field appropriately, making sure to set Type (C/P/W/O/F/G) = P and entering the appropriate Default Plan code. A category for Huntington Provider Group may look like the following example:
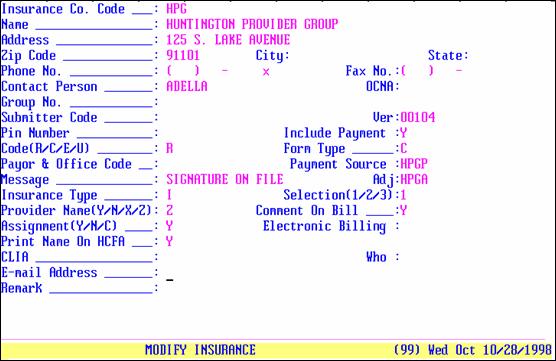
/Utility/Insurance:
Add an insurance company for each Capitated Contract. For more detailed reports, you may enter each insurance that may be part of this Capitated contract. For instance, within the Huntington Provider group patient’s may have Secure Horizons, PacifiCare, Blue Cross California Care, etc. To group these together, the name might be Secure Horizons HPG, PacifiCare HPG, etc. An insurance screen for Huntington Provider group may look like the following example:
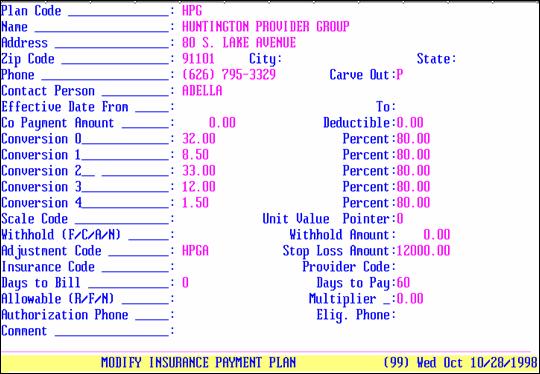
/Utility/Insurance/Pay Plan/Pay Plan:
Set up pay plans for the various contracts. A pay plan for Huntington Provider Group may look like the following example:
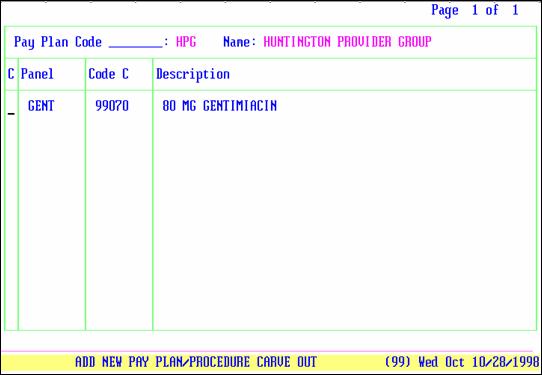
/Utility/Insurance/Pay Plan/Pay Plan/Procedure:
For each Capitated Pay Plan, for each Plan Code, enter each fee for service procedure here. Entering procedures here, which, per contract, will be paid at fee for service, tells On-Staff NOT to capture these particular procedures when using the Auto Payment feature. Their /Procedure screen’s HMO Adjust field MUST BE set to N in order for this area to exclude those procedures from the Auto Payment feature. If a procedure screen’s HMO Adjust is set to Y, entry in this area has no effect. That procedure will be written off at the time of posting when a patient has a pre-paid category type. A Pay Plan Procedure screen for Huntington Provider Group may look like the following example:
The /Utility/Insurance/Pay Plan/Pay Plan/Diagnosis screen allows you to carve out as fee for service all posted charges based on the diagnosis. When appropriate, enter those diagnoses.
/Utility/Procedure:
To allow flexibility between contracts, it is recommended to set ALL procedure’s HMO Adjust field to N, even though you may have a contract that you DO want the charge amount adjusted at the time of posting. See the following example:
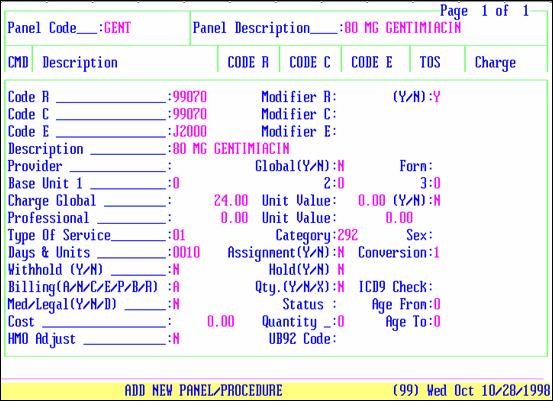
HMO Adjust: N
At the time of posting, a procedure whose HMO Adjust is N sets an internal flag which tells On-Staff that this procedure should be captured when doing auto payment. To allow flexibility between contracts, it is recommended to set ALL procedure’s HMO Adjust field to N. Then, per contract, fee for service procedures will be exclude through /Insurance/Pay Plan/Pay Plan/Procedure and contracts which the charge amount is to be adjusted at the time of posting will be determined by setting up their /Insurance/Pay Plan/Pay Plan <Withhold (F/C/A/N)> = C and <Withhold Amount> = 100 as well as the /Utility/Procedure <Withhold (Y/N)> = Y.
HMO Adjust: X
At the time of posting, a procedure whose HMO Adjust is X sets an internal flag which tells On-Staff that this procedure should NOT be captured when doing auto payment. To allow flexibility between contracts, it is recommended to set ALL procedure’s HMO Adjust field to N. Thus, for all procedures that will be paid as fee for service (thus payments will be made through Open Item Payment NOT Auto Payment) add them at /Insurance/Pay Plan/Pay Plan /Procedure.
HMO Adjust: Y
At the time of posting, a procedure whose HMO Adjust is Y tells On-Staff to automatically adjust the charge amount. It is not recommended to use Y:
a) This limits contract set up. Once this field has been set to Y and posting has begun, YOU MAY NOT CHANGE THE VALUE!
b) You may NOT exclude procedures through /Insurance/Pay Plan/Pay Plan /Procedure.
c) You may NOT use the Auto Payment feature for another contract.
To allow flexibility between contracts, it is recommended to set ALL procedure’s HMO Adjust field to N. Then, per contract, fee for service procedures will be exclude through /Insurance/Pay Plan/Pay Plan/Procedure and contracts which the charge amount is to be adjusted at the time of posting will be determined by setting up their /Insurance/Pay Plan/Pay Plan <Withhold (F/C/A/N)> = C and <Withhold Amount> = 100 as well as the /Utility/Procedure <Withhold (Y/N)> = Y (for ones that are to be written off, N for ones that are NOT to be written off).
NOTE: Using the Procedure’s Withhold (Y/N) in this fashion is assuming you will NOT be setting up any contract withhold amounts.
Optional - Creating a Copay Charge
From time to time, patients do not pay their copay at the time of service. Due to the nature of the program, you may choose to add a Copay procedure which will allow a statement to be printed for the unpaid copays as well as prevent the unpaid amount from being written off at the time of posting should the insurance pay prior to the patient. This charge will NOT bill out electronically nor on paper. Having a copay charge will allow front desk to collect AND post copays without needing the expertise of a biller, printing a journal to balance money received with money posted.
Example Copay Charge:
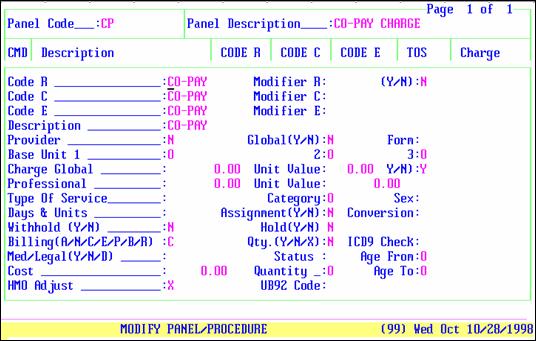
The following fields of a copay charge screen MUST be set as follows:
HMO Adjust: X
At the time of posting, this sets an internal flag which alerts On-Staff that these charges will be paid through Open Item Payment NOT Auto Payment.
Billing: C
At the time of posting, this defaults the Who column to G as the patient IS responsible for paying their co-payment, NOT their primary insurance. C alerts On-Staff to allow this charge to appear on the patient’s statement but NOT allow it to be billed electronically or on paper.
POSTING CHARGES
Post charges as usual. When all software requirements are in place and the patient’s demographic information has been entered correctly prior to posting charges:
When a charge is to be written off at the time of posting, the charge screen will request you to do so if you forget to commit the adjustment prior to exiting the charge screen.
When a charge is to be captured for the Auto Payment feature, this will be automatically flagged behind the scenes at the time of posting.
When a charge is contracted as fee for service (payment being received on a separate check), this will be automatically flagged behind the scenes at the time of posting and the system will not allow that charge to be captured at the time of posting the cap check through Auto Payment. Payment for fee for service charges will be posted through Open Item Payment.
If you have chosen to post a copay charge, for consistency it is recommended to do so for ALL patient’s.