OnSTAFF 2000
/Management/Reports/Detail
DETAIL REPORTS
Detail Reports display requested information as it was at the time of posting the charge. These reports are accessible through the /Management/Reports Menu by selecting the Detail menu option.
C The Detail Procedure Report gives Patient Account Number, Name, Category, Place of Service, Referring, Insurance, Date of Service, Posting Date, Code, Modifier, Charge, Approved, Payment, Adjustment, Who, and Totals on charges, approved, payments, and adjustments. Instructions for requesting this report are detailed on the following pages. Following are a few benefits:
· The report could list patients who had charges entered for that day, totaling those charges as well as any payments posted that day towards those charges.
· The report could provide a report of patients whose balance is still due from their secondary insurance companies based on a specified last payment date.
· The report could provide a report for a specific procedure noting the approved, payment, adjustment, and charge amount(s) sorting this by insurance.
· The report could provide a report for all charges still on 'Hold' status (/Ledger <W> (Who column) still equals Y).
D The Diagnosis Report gives Patient Account Number, Name, Category, Phone, Date of Service, ICD9 Code, and Description and is followed by the Summary Diagnosis Report and may be requested for a specific date range, a specific provider, category, sex, age from and to range, CPT Code, ICD9 Code (i.e., 949.5, or by using the asterisk, 94*, to include all ICD9 codes that begin with ‘94’), facility, insurance or referring. Instructions for requesting this report are detailed on the following pages. Following are a few benefits:
· The report could list all patients with the specified ICD9, insurance, and CPT Code in order to correct an incorrect ICD9 and rebill.
· The report could list all patients with diagnosis ____ between the ages of ___ and ___ for a drug rep with a new drug.
· The report could list all patients with ___ so they can be informed of a new laser technique to correct ___.
Requesting Report Code L, using the same criteria, will print mailing labels for the selected patients. Requesting Report Code F, using the same criteria, will print a letter addressed to the selected patients.
S The Summary Report is the same report as Report Code D, the Diagnosis Report, but summarizes the information. For example, if one patient has several dates of service within the requested date range for the requested diagnosis, the Summary Report will print only one line of information corresponding to the date of service of the last entered charge for the most current entry date that falls within the requested dates of service.
L Report Code L will print patient mailing labels for the patients selected in the Diagnosis Report (Report Code D) and so must be requested using the same criteria (field entries) used to request Report Code D.
F Report Code F will print a letter for the patients selected in the Diagnosis Report (Report Code D) and so must be requested using the same criteria (field entries) used to request Report Code D. Contact the Software Department for a customized letter.
Using /Management/Report/Detail Date Fields (<From Date> and <To Date>, <Date From> and <To Date>)
Report Code C
The first set of dates (<From Date> and <To Date> fields):
Are entry, service, last payment or first billing date(s) of the charges.
The second set of dates (<Date From> and <To Date> fields):
Are always the entry date(s) of payments and adjustments posted against the charges specified in the first set of dates, or when left blank, ALL payments and adjustments posted to date against the charges specified in the first set of dates. The report will contain payment and adjustment details when the second set of date fields are used, or when left blank, will summarize charge payment and adjustment.
Report Codes D, S, L, F
The first set of dates (<From Date> and <To Date> fields):
Are always the entry date(s) of the charges associated with the requested diagnosis(es) (<Date Selection> must always be E).
The second set of dates (<Date From> and <To Date> fields):
Are always the service date(s) of those charges associated with the requested diagnosis(es) entered during the first set of dates.
Why the two dates? Some charges such as hospital consults or a missing charge ticket may not have been posted during the month in which they occurred. For example, to include ALL information for the month of March (regardless of their entry date), complete the first set of date fields as follows:
The first set of dates define the entry date(s) of the charges associated with the requested diagnosis(es):
<From Date> 03/01/2000
<To Date> 08/05/2000 (enter T for today's calendar date)
The second set of dates define the service date(s) of ONLY those charges selected as a result of the first set of dates above, associated with the requested diagnosis(es):
<Date From> 03/01/2000
<To Date> 03/31/2000
Management/Reports/Detail
Selecting the Detail option from the /Management/Reports Menu will display the following screen:
\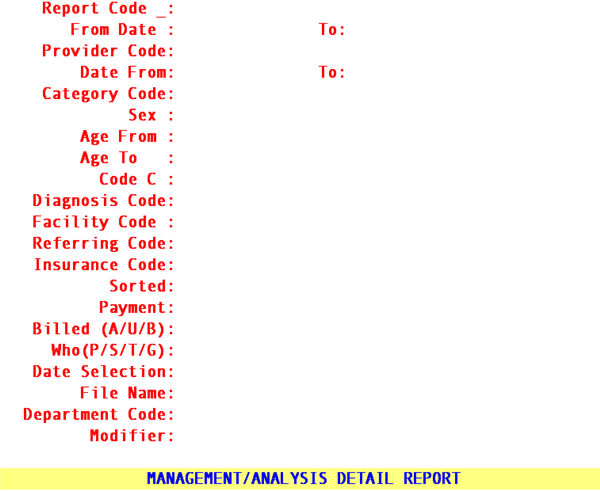
Instructions for requesting reports are as follows:
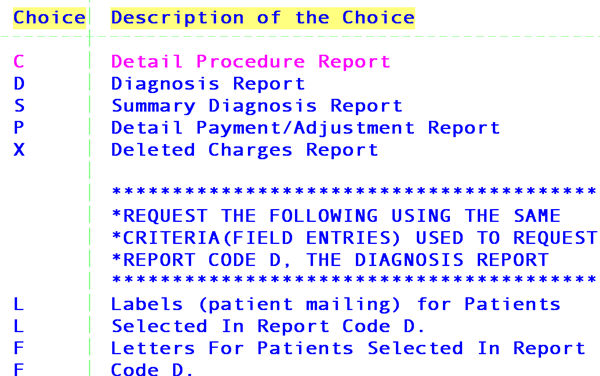
Report Code: Press [F2] on the <Report Code> field to display the following report options:
S Summary Report
L Mailing Labels (must be requested using the same criteria (field entries) used to request Report Code D).
F Letters (must be requested using the same criteria (field entries) used to request Report Code D).
From Date:
To Date: Report Code: C
These dates identify the entry, service, last payment or first billing date of the charges as determined by the <Date Selection> field entry.
Report Code: D, S, L, F
These dates define the entry date(s) of the requested information. (Remember to enter a wide range of entry dates. The second set of dates will define the time period.)
NOTE: When more than one date of service is posted during the same charge session only the first charge date will be printed on the report.
Provider
Code: Report Code: C, D, S, L, F (all report codes)
Press [Enter] to include all providers. To request the report for a specific provider enter their /Utility/Provider <Provider Code>.
Date From:
To Date: Report Code: C
These dates are always the entry date(s) of ALL payments and adjustments (NOT ONLY those related to the charges identified in the first set of dates) or when left blank, ALL payments and adjustments but ONLY those related to the charges identified in the first set of dates regardless of when they were posted.
NOTE: ONLY when dates are entered in the second set of date fields, will payment and adjustment detail, per charge, be printed.
Report Code: D, S, L, F
These dates identify the date of service(s) of those charges posted within the entry date(s) specified in the first set of dates.
Category
Code: Report Code: C, D, S, L, F (all report codes)
Press [Enter] to include all categories. To request the report for a specific category, enter the /Utility/Category <Category Code>.
NOTE: The report includes this information based on the category assigned to the patient at the time of posting charges, which may not be, at the time of running the report, the patient's current category.
Sex: Report Code: C, D, F, L, S (all report codes)
Press [Enter] to include both males and females. To request the report for a specific sex, enter:
M - limit the report to males
F - limit the report to females
Age From: Report Code: C, D, S, L, F (all report codes)
Press [Enter] to include all ages. To request the report for a specific age or age range, enter the beginning age in whole years only.*
Age To: Report Code: C, D, S, L, F (all report codes)
Press [Enter] to include all ages. To request the report for a specific age or age range, enter the ending age in whole years only.*
NOTE: The report includes this information based on the age of the patient at the time of posting.
Code C: Report Code: C
Enter the /Utility/Procedure <Code C> of the procedure.
To request the report for a specific CPT Code pertaining to the requested diagnosis, enter the /Utility/Procedure <Code C> value. Otherwise, press [Enter].
NOTE: In most cases, /Utility/Procedure <Code C> is the field used for CPT Coding. Whether this is your case or not, the report looks to this field ONLY for it's Panel Code criteria. Keep in mind procedures with HCPCs (usually entered on Code E) and X codes (usually entered on Code R) will need to have the Code C value entered on this field in order for this to be captured in the report. Printing a procedure listing from /Utility/Procedure/Print will list Code R, C, and E for you.
Diagnosis Code: NOTE: Enter the value found in the /Utility/Diagnosis <Diagnosis Code> field, NOT the actual diagnosis code found in the /Utility/Diagnosis <ICD9 Code> field. Although reports D, F, L, and S are requested by the /Utility/Diagnosis <Diagnosis Code> the report displays the <ICD9 Code> field. In most cases, both field values are the same with the exception of speed coded diagnoses on a SuperBill.
Report Code: C
NOT USED.
Report Code: D, L, F
Enter the /Utility/Diagnosis <Diagnosis Code> to request the report for only one diagnosis. The asterisk (*) may be used in requesting the criteria. For example, to request a report for each /Utility/Diagnosis <Diagnosis Code> within the 940 series enter 94*.
Report Code: S
Enter the /Utility/Diagnosis <Diagnosis Code> to request the report for only one diagnosis. The asterisk (*) is NOT USED with Report Code C.
Facility Code: Report Code: C, D, S, L, F (all report codes)
Press [Enter] to include all facilities. To request the report for a specific facility, enter the desired /Utility/Facility <Facility Code>.
Referring Code: Report Code: C, D, S, L, F (all report codes)
Press [Enter] to include all referrals. To request the report for a specific referral source, enter the desired /Utility/Referring <Referring Code>.
Insurance Code: Report Code: C, D, S, L, F (all report codes)
Press [Enter] to include all primary insurance carriers. To request the report for a specific primary carrier, enter the desired /Utility/Insurance <Insurance Code>.
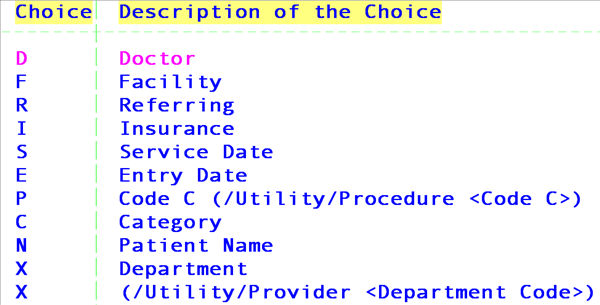
Sorted: Report Code: C
This field will default to the /Utility/Set Up/Parameter <Entry/Service Date(E/S)> field entry (usually E). Pressing the F2 search key will display the following valid choices:
Report Code: D, S, L, F
NOT USED. The program sorts automatically in descending account number order. Press [Enter] to bypass this field.
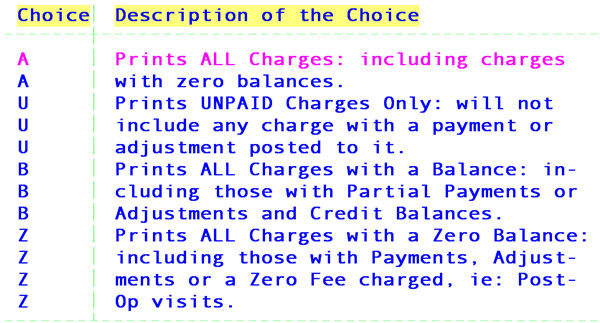
Payment(A/U): Report Code: C
This field defaults to A automatically and allows you to request the report for all charges or only unpaid charges. Pressing the [F2] search key will display the following valid choices:
Report Code: D, S, L, F
NOT USED.
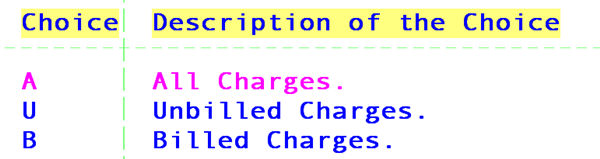
Billed(A/U/B): Report Code: C
This field defaults to A automatically and allows you to request the report for all, unbilled or billed charges. Pressing the [F2] search key will display the following valid choices:
Report Code: D, S, L, F
NOT USED.
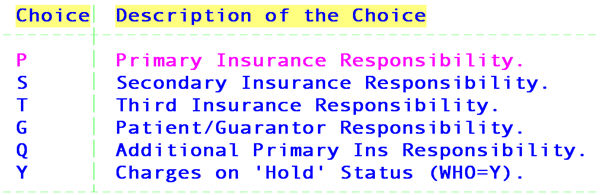
Who(P/S/T/G): Report Code: C
This field defaults to * automatically and allows you to request the report based on how the charge is marked in the patient's /Ledger/Accounting or Open Item <W> (WHO) column. Pressing the [F2]search key will display the following valid choices:
Report Code: D, S, L, F
NOT USED.
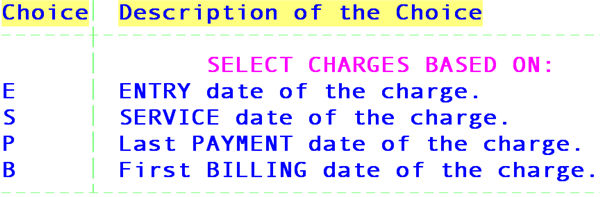
Date Selection: Report Code: C
This field will default to the /Utility/Set Up/Parameter <Entry/Service Date(E/S)> field entry (usually E). Pressing the [F2] search key will display the following valid choices:
Report Code: D, S, L, F
E - ALWAYS
File Name: Report Code: C, D, S
NOT USED.
Report Code: L
This field will default to PcsLabel, the file name for mailing labels for patients.
Report Code: F
Pressing the F2 search key will display the following valid choices:
DLC Detail Letter for billing method by Clinic (C).
DLD Detail Letter for billing method by Doctor (D).
Department Code For all code types the default is all departments (leave blank).To request the report for a specific department, type the Utility --►Provider <Department > name or number.
Modifier Press enter for this report to include ALL charges (with or without modifiers). Enter a specific modifier (e.g. YB or 28), OR enter 5*, for example, to include all modifiers that begin with 5.
ABOUT REPORT CODE C PRINTED REPORT
Report Title: DETAIL PROCEDURE REPORT
Account: Patient account number.
Name: Patient name.
Cat: The /Utility/Category <Category Code>assigned to the patient at the time of posting charges, which may be different than the patient's current category.
POS:* The /Utility/Facility <Facility Code> (place of service) used at the time of posting charges.
Referring: The /Utility/Referring <Referring Code> at the time of posting charges, as follows:
If /Utility/Set Up/Parameter <Referring (P/C/F)> = P,
the /New Patient <Referral> entry will print (see NOTE).
If /Utility/Set Up/Parameter <Referring (P/C/F)> = C,
the /Charges/Charge <Rdr.> entry at the time of posting charges will print (see NOTE).
If /Utility/Set Up/Parameter <Referring (P/C/F)> = F,
On-Staff first checks the /Charges/Charge <Rdr.> entry and if blank, then the /New Patient <Referral> entry will print (see NOTE).
NOTE: ONLY when /Utility/Referring <Doctor/Other (D/O)> = D
Insurance: The /Utility/Insurance <Insurance Code> assigned to the patient at the time of posting charges, which may be different than the patient's current insurance.
DOS: The date of service of the charge.
Posting Date:* On-Staff's entry date at the time of posting charges.
Code:* The /Utility/Procedure <Code C> for the Panel Code used at the time of posting charges.
Mod: The /Charges/Charge <Mod.> (modifier) used at the time of posting charges.
Charge: The /Charges/Charge <Charge> (charge amount) at the time of posting charges.
Approved: If a fee schedule is involved, Approved will print that fee schedule’s /Utility/Procedure/Fee Schedule <Approved> amount.
* When requesting the report and dates are entered in the second set of date fields:
· The payment description will print following the charge under the POS heading (/Utility/Messages /Remark <Description> of the <Remark Code> used in the /Payment/Open_Item <S_Pay> field to define the payment at the time of posting).
· The entry date of the payment (or adjustment) will print following the charge under the Posting Date heading.
· The remark code will print following the charge under the Code heading (/Utility/Messages/Remark <Remark Code> used in the /Payment/Open_Item <S_Adj> field to define the adjustment at the time of posting).
If conversion rate/unit value set up is involved, Approved will print the contract approved amount by multiplying the conversion rate times the unit value for the noted procedure. For further information regarding conversion rate/unit value set up, see Session II Training Documentation Software Requirements for Contract Set Up provided during your initial training.
When neither is involved, Approved will print the /Utility/Procedure <Charge Global> amount.
Payment: The /Utility/Messages/Remark <Description> of the <Remark Code> used in the /Payment/Open_Item <S_Pay> field at the time of posting payments.
Adjustment: The /Utility/Messages/Remark <Description> of the <Remark Code> used in the /Payment/Open_Item <S_Adj> field at the time of posting adjustments.
Who: The /Ledger (either Accounting or Open Item) <W> (Who) column value at the time of running the report.
ABOUT REPORT CODE D PRINTED REPORT
First part of the report:
Report Title: DIAGNOSIS REPORT
Account: Patient account number.
Name: Patient name.
Cat: The /Utility/Category <Category Code>assigned to the patient at the time of posting charges, which may be different than the patient's current category.
Phone: The /New Patient <Home Phone No.> of the patient.
DOS: The date(s) of service related to the requested diagnosis code(s).
NOTE: When more than one date of service is posted during the same charge session only the first charge date will be noted on the printed report.
ICD9: The /Utility/Diagnosis <ICD9 Code> for the requested /Utility/Diagnosis <Diagnosis Code(s)>.
Description: The /Utility/Diagnosis <Description> for the requested /Utility/Diagnosis <Diagnosis Code(s)>.
Second part of the report:
Report Title: SUMMARY DIAGNOSIS REPORT
CODE: The /Utility/Category <Category Code> assigned to the patient at the time the charges were posted, which may be different than the patient's current category.
DESCRIPTION: The /Utility/Category <Description> for the associated /Utility/Category <Category Code>.
PATIENT COUNT: The number of patients within the specified category that match the requested criteria.
%: The percent of the report item’s PATIENT COUNT to the overall total for that column. (Percent (%) is ALWAYS in reference to the information in the previous column.)
ABOUT REPORT CODE S PRINTED REPORT
The printed Report Code S is the same as Report Code D.
ABOUT PRINTED CODE L
Report Code L prints mailing labels (two columns) for patients. Remember, this report must be requested using the same criteria (field entries) used to request Report Code D.
ABOUT PRINTED CODE F
Report Code F prints a letter to patients based on the selected criteria. Remember, this report must be requested using the same criteria (field entries) used to request Report Code D.
If you currently have letterhead printing on your follow up and recall letters and would like it also on the letter that prints here, contact the Software Support Department.
If you would like additional letters or would like this letter changed, contact the Software Support Department.
.