
Intellect™
CHARGES MENU OPTIONS

PM 160 Review
When Phase 2 of the CHDP Transition to National Standards is effective for dates of service ON or AFTER July 1, 2017, the PM 160 will no longer be used for submitting CHDP claims. This documentation is only applicable for CHDP set up and charge posting for dates of service PRIOR to July 1, 2017. Please refer to Charges --►CHDP--►Transition to National Standards documentation for posting dates of service on or after July 1, 2017.
See also additional information from Medi-Cal website: CHDP Frequently Asked Questions
The CHDP menu option is used to post all assessment and immunization charges for a qualifying child under the State of California - Child, Health and Disability Prevention (CHDP) program and generate the PM 160 CONFIDENTIAL SCREENING/BILLING REPORT.
This document shows where the information is pulled from in Intellect to fill the PM 160 boxes. This document is grouped into sections that correlate to sections on the PM 160:
CHDP Assessment Screening Procedures and Codes
Patient Eligibility (Standard PM 160)
The Questions Below Must Be Answered
Note: Before using the CHDP option, set up is required. See CHDP Set Up for details.
See also Critical Denial Codes.
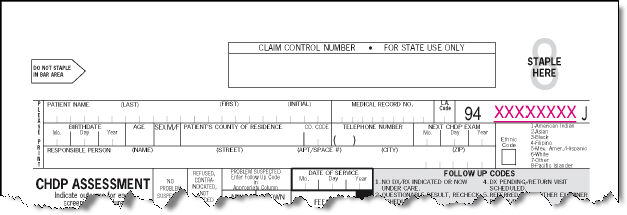
Patient Name:
Pulled from Registration --►Regular --►Patient <Last Name>, <First Name>, <Middle Initial>.
Medical Record Number:
Pulled from Registration --►Regular --►Patient <Patient Account No.>.

L.A. Code:
Pulled from Charges --►CHDP <LA Code>.
Use for Los Angeles County only.
Pre-Imprinted Field:
This field is pre-imprinted with a form control number that begins with '94' and ends with either 'J' or 'K.'

Birthdate:
Pulled from Registration --►Regular --►Patient <DOB>

Age:
Intellect computes the patient's age for the Date of Service based on Registration --►Regular --►Patient <DOB>
It is formatted with one of the following indicators: 'y' for years, 'm' for months, 'w' for weeks, or 'd' for days (for example, 15y represents 15 years of age).
Note: If the patient’s date of birth needs to be changed on the demographic screen AFTER charges are posted, delete the CHDP charges and repost them. Failure to do so results in an incorrect age printing on the CHDP form if the claim is printed after the date of birth is corrected. This applies ONLY to CHDP charges, not any other type of charges.

Sex:
Pulled from Registration --►Regular --►Patient <Gender>
Note: Sex must be entered exactly as it appears on the Medi-Cal eligibility verification system. If the sex stated on the Medi-Cal eligibility verification system is incorrect, note this in the Comments/ Problems area.
Patient's County of Residence and Code:
Pulled from Registration --►Regular --►Patient
Intellect completes the county and county code based on the Registration --►Regular --►Patient <Zip Code> for the patient's home address.
Telephone Number:
Pulled from Registration --►Regular --►Patient <Home Phone NO.>
Next CHDP Exam:
Intellect computes this based on the DOS OR it is the date entered Charges --►CHDP <Next Visit>
It is the month and year of the next appointment for children 3 years of age and older.
Responsible Person Name and Address:
Based on Registration --►Regular --►Patient <Guarantor>, the following information is pulled from the Guarantor's account:
Registration --►Regular --►Patient <Guarantor Name>
Registration --►Regular --►Patient <Address>
Registration --►Regular --►Patient <City>
Registration --►Regular --►Patient <State>
Registration --►Regular --►Patient <Zip Code>
Ethnic Code:
Pulled from Registration --►Regular --►Patient <Ethnicity>
Date of Service:
Pulled from Charges --►CHDP <DOS>
CHDP Assessment Screening Procedures and Codes
Screening procedure codes 01 through 12 are pre-printed on the form. Column A, B, C, and D are populated for any procedure where Utility--►Procedure--►Procedure <CHDP> = A.

Column A No Problem Suspected:
Pulled from Charges --►CHDP <A/B>
Type an 'A' In this column to select the procedure. Intellect places an 'X' in the indicated column for the appropriate procedure.

Column B Refused, Contraindicated , Not Needed:
Pulled from Charges --►CHDP <A/B>
Type a 'B' In this column to select the procedure. Intellect places an 'X' in the indicated column for the appropriate procedure.
Column C New:
Pulled from Charges --►CHDP <C>
Type a Follow up Code Number in this column to select the procedure. Intellect places an 'X' in the indicated column for the appropriate procedure.
Note: If the sequence number of a procedure is '01,' then the 'C' Column accepts two follow up codes separated by a comma.
Column D Known:
Pulled from Charges --►CHDP <D>
Type a Follow up Code Number in this column to select the procedure. Intellect places an 'X' in the indicated column for the appropriate procedure.
Note: if the sequence number of a procedure is '01', then the 'D' Column accepts two follow up codes separated by a comma.
Other Tests:
Pulled from Charges --►CHDP
For any procedures where Utility --►Procedure --►Procedure <CHDP> = A
AND Utility --►Procedure --►Procedure <CHDP Seq> is greater than ‘12’
AND Charges --► CHDP <A/B>, <C>, or <D> has an entry.
The following prints:
• CODE: Utility --►Procedure --►Procedure <CHDP Seq>
• OTHER TESTS: Utility--► Procedure --► Procedure <Description>
• For columns A, B, C & D see above.
Pulled from Charges --►CHDP <Height>
Pulled from Charges --►CHDP <Weight>
Body Mass Index (BMI) Percentile:
Intellect computes the Body Mass Index (BMI) PERCENTILE based on the Charges --►CHDP <Height> and Charges --►CHDP <Weight>
Pulled from Charges --►CHDP <BP Syst>
and Charges --►CHDP <BP Diast>
Pulled from Charges --►CHDP <HGB>
Pulled from Charges --►CHDP <HCT >
Pulled from Charges --►CHDP <Birth Weight>
Birth weight should be entered for children younger than 2 years of age.
Pulled from Charges --►CHDP <A/B>
Utility --►Procedure --►Procedure <CHDP Seq> and <Description> print for all procedures where Utility --►Procedure --►Procedure <CHDP> = 'I' AND Charges --►CHDP <A/B> has an entry.

Column A - Now Up To Date for Age:
Pulled from Charges --►CHDP <A/B>
Type an 'A' in this column to select the procedure. Intellect places an 'X' in the indicated column for the appropriate Procedure.

Column B - Still Not Up To Date for Age:
Pulled from Charges --►CHDP <A/B>
Type a 'B' in this column to select the procedure. Intellect places an 'X' in the indicated column for the appropriate Procedure.

Column C - Already Up To Date for Age:
Pulled from Charges --►CHDP <A/B>
Type a 'C' in this column to select the procedure. Intellect places an 'X' in the indicated column for the appropriate Procedure.

Column D - Refused or Contraindicated:
Pulled from Charges --►CHDP <A/B>
Type a 'D' in this column to select the procedure. Intellect places an 'X' in the indicated column for the appropriate Procedure.
Patient Visit:
Pulled from Charges --►CHDP <Patient Visit>
Type of Screen:
Pulled from Charges --►CHDP <Type of Screen>
Fees:
Fees do not apply to the PM 160 Information -- only the claim form.
Charges --►CHDP <Charge>:
• The fees populate for Assessments where Utility --► Procedure--► Procedure <CHDP> = 'A' AND Charges --►CHDP <A/B> = A or there is an entry in <C> or <D>.
• The fees populate for Immunizations where Utility --► Procedure--► Procedure <CHDP> = 'I' AND Charges --►CHDP <A/B> is A or B.
The Charges --►CHDP <Charge> pulls from:
• Utility --► Procedure--► Procedure <Charge Global> field IF a fee schedule is NOT set up for the provider, insurance company and panel code OR the Utility --► Insurance--► Pay Plan--► Pay Plan <Plan Code> in <Pay Plan> field on the patient's insurance screen.
• Utility --► Procedure--► Fee Schedule <Alt. Charge> field IF a fee schedule IS set up for the provider, insurance company and panel code OR the Utility --► Insurance--► Pay Plan--► Pay Plan <Plan Code> in <Pay Plan> field on the patient's insurance screen.
Total Fees:
Pulled from Charges --►CHDP <Total Charge>
Intellect calculates the total of the fees for all CHDP Assessments, Other Tests, and Immunizations.
Service Location
Service Location:
The Provider code entered in Charges--►CHDP <Billing Provider> determines:
• Line 1: Utility --►Provider --►Provider <Organization Name>. If <Organization Name> is blank, the Provider's name prints.
• Line 2: Utility --►Provider --►Provider <Address>.
• Line 3: Utility --►Provider --►Provider <City>, <State>, <Zip Code>, <Phone Number>.
For CHDP billing in Intellect, only one NPI number is submitted. Depending on how the clinic is registered, bill using either the Group NPI or Individual Provider NPI.
When setting up, always add a Provider --►Provider or Provider --►Facility record with the required NPI number in the Group NPI field, even if the clinic bills with the Individual Provider NPI.
For the [Provider Number] field, Intellect prints the NPI number for the provider code entered in Charges --►CHDP <Billing Provider> based on the hierarchy:
• Intellect first looks in Utility --►Provider --►Provider Facility <Group NPI> for a match to the Billing Provider, Insurance, and Facility.
• If a match is not found in the Provider Facility screen, the program looks to Utility --►Provider --►Provider Provider <Group NPI> for a match to the Billing Provider and Insurance Code.
• If a match is not found in the Provider Provider screen, the program looks to Utility --►Provider --►Provider <Group NPI> for the Billing Provider
Place of Service:
Prints the Utility --►Facility <Place of Service> for the facility code entered in Charges --►CHDP <Facility>
Signature of Provider:
Dr or a designated representative must sign and date the PM 160 or PM 160 Information Only claim form. Do not use a signature stamp.
Referred To:
Prints the Utility --► Referring <First Name> <Middle Initial> <Last Name> <Title> for the Referring Code entered in the first Charges --►CHDP <Referring> field.
Telephone Number:
Prints the Utility --► Referring <Phone No> for the Referring Code entered in the first Charges --►CHDP <Referring> field.
Referred To:
Prints the Utility --► Referring <First Name> <Middle Initial> <Last Name> <Title> for the Referring Code entered in the second Charges --►CHDP <Referring> field.
Telephone Number:
Prints the Utility --► Referring <Phone No> for the Referring Code entered in the second Charges --►CHDP <Referring> field.
Comments/Problems:
Pulled from Charges --►CHDP <Comments/ Problems>
Following are examples of information to include when appropriate:
• The reason(s) for performing Medically Necessary Interperiodic Health Assessments (MNIHAs). Required in this field: A comment explaining the reason that a service was performed, even if the need for a MNIHA was identified at the time of the Gateway transaction.
• Diagnosis and related IDC-9 code, if a diagnosis is made during the visit.
• Explanation of suspected problems; for example, the nature of a dental problem. Identify dental problems using the 'Classification of Dental Treatment Needs', Classes II–IV. See the American Dental Association’s 'Classification of Treatment Needs' in the Appendix of their manual.
• Identify whether a patient 3 years of age or older is receiving (or the last time received) dental care.
• Explain when a procedure is not performed when the procedure is listed as recommended for age. (See the Periodicity Schedule for Health Assessment Requirements by Age Groups table in the Appendix of this manual). This includes tests that are performed at an age younger than the age specified.
• Record the screening procedure code and the name and telephone number of the referred provider when more than two referrals are made.
• Document the head circumference measurement for children 2 years of age or younger. Record measurements to one-fourth (1/4) inch.
• Results of vision test.
• Results of blood lead tests, when known.
• Primary language of the patient or guardian if other than English.
• Patient did not return for the reading of a Tuberculin (TB) test.
• NOTE discrepancies between known information and information provided by the eligibility verification system; for example, gender.
• Mother's Medi-Cal identification number is being used to bill for services rendered to an infant during the birth month or the month following.
• The reason for extra time spent with the patient when billing for an 'Extended Visit' for other than new patients or patients not assessed within the last two years.
• Immunization administered because individual is in a high-risk category.
• Elevated blood lead levels.
• Results of blood glucose test and whether the results are within normal limits.
• Results of cholesterol test and whether the results are within normal limits.
Routine Referrals - Blood Lead:
If Charges --►CHDP <Blood Lead> is 'Y,' then Intellect places an 'X' in the BLOOD LEAD box.
Routine Referrals - Dental:
If Charges --►CHDP <Dental> is 'Y,' then Intellect places an 'X' in the DENTAL box.
If Charges --►CHDP <Foster Child> is 'Y,' then Intellect places an 'X' in the PATIENT IS A FOSTER CHILD box.
Diagnosis Codes:
DIAGNOSIS CODE 1: Prints the first Charges --►CHDP <ICD9 Code>.
DIAGNOSIS CODE 2: Prints the second Charges --►CHDP <ICD9 Code>.
The Questions Below Must Be Answered
1. Patient is exposed to passive (second-hand) tobacco smoke?
• If Charges --►CHDP <Passive Smoke> is 'Y,' then Intellect places an 'X' in the Yes box.
• If Charges --►CHDP <Passive Smoke> is 'N,' then Intellect places an 'X' in the No box.
2. Tobacco used by patient?
• If Charges --►CHDP <Tobacco Use> is 'Y,' then Intellect places an 'X' in the Yes box.
• If Charges --►CHDP <Tobacco Use> is 'N,' then Intellect places an 'X' in the No box.
3. Patient counseled about/referred for tobacco use prevention/cessation?
• If Charges --►CHDP <Counseled> is 'Y,' then Intellect places an 'X' in the Yes box.
• If Charges --►CHDP <Counseled> is 'N,' then Intellect places an 'X' in the No box.
WIC Status
Charges --►CHDP <WIC Referral>:
• If Charges --►CHDP <WIC Referral> is 'Enrolled,' then Intellect places an 'X' in box 1 for 'Enrolled in WIC'.
• If Charges --►CHDP <WIC Referral> is 'Referred,' then Intellect places an 'X' in box 2 for 'Referred to WIC'.
• If Charges --►CHDP <WIC Referral> is blank, then neither box is marked.
Partial Screen
and
Screening Procedure ReCheck:
Charges --►CHDP <Screening>:
• If Charges --►CHDP <Screening> is 'Partial,' then Intellect places an 'X' in box 1 for PARTIAL SCREEN.
• If Charges --►CHDP <Screening> is 'Recheck,' then Intellect places an 'X' in box 2 for SCREENING PROCEDURE RECHECK.
• If Charges --►CHDP <Screening> is blank, then neither box is marked.

Accompanies prior PM 160 Dated:
Pulled from Charges --►CHDP < Prior Pm 160 Dated>
Patient Eligibility (Standard PM 160)

County:
Intellect completes the county code based on the Registration --►Regular --►Patient <Zip Code> for the patient's home address.
See CHDP Patients Add County Code for additional information.

Aid:
Charges --►CHDP <Aid>
Identification Number:
Pulled from Registration --►Regular --►Patient --►Insurance <Subscriber No.>
For the insurance-billed Charges --►CHDP <Insurance>
This must be the patient's Medi-Cal Identification number not a Social Security number.
Use of BIC for Billing Now Required
Effective for dates of service on or after February 1, 2008, providers billing for CHDP services using the standard Confidential Screening/Billing Report (PM 160) are prohibited from using a Social Security Number (SSN) when entering the client's identification number in the Patient Eligibility portion of the form. Providers are required to use either the nine-digit Client Index Number (CIN) or the 14-character Medi-Cal identification number from the client's Benefits Identification Card (BIC), paper ID card or TriZetto (formerly Gateway) transmittal document. The 14-character ID number is located on the front of the BIC card and consists of a nine-digit CIN, a Check Digit, and a 4-digit issue date. The issue date is used to deactivate cards that have been reported as lost or stolen.
Patient Eligibility (Check Boxes):
Charges --►CHDP < Pt Elig >:
• If Charges --►CHDP <Pt Elig> is '1,' then Intellect places an 'X' in box 1 for 'If covered by Medi-Cal, or pre-enrolled in CHDP Gateway, enter BIC number'.
• If Charges --►CHDP <Pt Elig> is '2,' then Intellect places an 'X' in box 2 for 'Patient eligible for CHDP benefits only'.
• If Charges --►CHDP <Pt Elig> is blank, then neither box is marked.