
Intellect™
CHARGES MENU OPTIONS

CHDP Transition to National Standards
Child Health and Disability Prevention (CHDP) program is transitioning claims submission from PM160 to the national standards for paper claims (CMS1500 or UB04) and electronic equivalent.
• Phase 1: Transitions clinical laboratory-only services effective for dates on or after February 1, 2017.
• Phase 2: Transitions the remaining CHDP services (including assessments & immunizations) effective for dates of services on or after July 1, 2017.
In this Topic:
What set up changes are needed?
For dates of service on or after July 1, 2017, CHDP well-child health assessments and immunizations are billed as Medi-Cal services under the Early and Periodic Screening, Diagnosis and Treatment (EPSDT) benefit.
• CPT and HCPCS codes with modifiers replace the two-digit CHDP codes. See the CHDP Program Code Conversion Table on the Medi-Cal website http://files.medi-cal.ca.gov/pubsdoco/newsroom/25768_Cd_Conv_Table.pdf
• CMS1500 or UB04 claim forms replace PM160 for paper claims.
• Providers are able to submit CHDP claims electronically through a clearinghouse. NOTE: Additional enrollment may be required to submit Medi-Cal claims through the clearinghouse of choice.
• In Intellect, charge posting is done through the Charges --►Charge screen.
See CHDP Frequently Asked Questions on the Medi-Cal website https://files.medi-cal.ca.gov/pubsdoco/chdp_faq.aspx
What set up changes are needed?
If the Charges --►CHDP screen was used to post charges for dates of service prior to July 1, 2017, then the following screens need to be reviewed BEFORE posting dates of service on or after July 1, 2017 on the Charges --►Charge screen:
1. Utility --►Procedure --►Procedure
Update existing panel codes with the CPT/HCPCS codes listed on the CHDP Program Code Conversion Table.
NOTE: Clinics using the same Panel Code for commercial insurances and the CHDP program, may not need to make any changes to this screen.
1.1 <Code R> (usually used for Medi-Cal insurances): Enter the appropriate CPT or HCPCS code NOT the two-digit CHDP code.
1.2 <Code C> (usually used for commercial insurances): Enter the appropriate CPT or HCPCS code NOT the two-digit CHDP code.
1.3 <Code E> (usually used for Medicare insurances): Enter the appropriate CPT or HCPCS code NOT the two-digit CHDP code.
1.4 <Age From> and <Age To>: If applicable, enter the age in YEARS.
1.5 <CHDP>, <CHDP Seq>, <CHDP Age From>, and <CHDP Age To>: These fields are no longer used for dates of service on or after 7/1/2017.
IMPORTANT: DO NOT REMOVE DATA. This information is required for billing dates of service prior to July 1, 2017 on PM160.
2. Utility --►Insurance --►Insurance
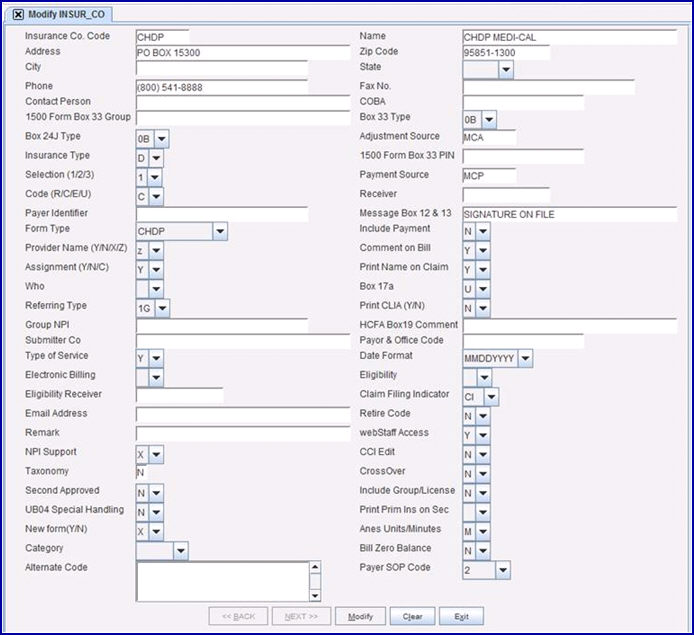
2.1 CHDP insurance: This is used for submitting claims for dates of service prior to July 1, 2017. NO CHANGES ARE REQUIRED. For example:
2.2 Medi-Cal insurance: Previously used for submitting all non-CHDP claims, this is also used to submit CHDP/EPSDT claims on or after July 1, 2017.
2.2.1 <Code (R/C/E/U)>: DO NOT CHANGE THIS FIELD. This field indicates if <Code R>, <Code C>, <Code E>, or <Code O> on the Utility --►Procedure --►Procedure screen is submitted when billing this insurance.
2.2.2 <Form Type>: Set to ‘NEW HCFA RED’ to print paper claims on the red & white CMS1500 form.
If claims are sent electronically through a clearinghouse, then the following fields may need to be updated after enrollment is completed:
2.2.3 <Receiver>: Enter the Medi-Cal Payer ID# from the clearinghouse Payer List.
2.2.4 <Payer Identifier>: Enter the Medi-Cal Payer ID# from the clearinghouse Payer List.
2.2.5 <Payor & Office Code>: Enter the Medi-Cal Payer ID# from the clearinghouse Payer List.
2.2.6 <Electronic Billing>: Enter the one-character code for the clearinghouse of choice. If unknown, please verify with a trainer or support.
3. Utility --►Procedure --►Fee Schedule
Payments are subject to Medi-Cal reimbursement rates. Clinics that track approved amounts and/or bill alternate fees for CHDP charges, need to add updated fee schedule entries effective 07/01/2017.
4. Registration --►Regular --►Patient --►Modify
Compliance with the billing national standards has eliminated some of the data entry requirements for the PM160. Please note:
4.1 Modify PATIENT screen
4.1.1 <Guarantor>:
It is no longer a billing requirement to include RESPONSIBLE PERSON on claims. However, the Guarantor account MUST be completed:
• If sending Family Statements or using the Pediatric Registration screen, then enter the Guarantor’s Account Number.
• If NOT sending Family Statements or using Pediatric Registration screen, enter the <Patient Account No.> for this patient.
4.1.2 <Zip Code>:
It is no longer a billing requirement to update the <County> and <County Code> in the zip code database. Note, the 5- or 9-digit zip code MUST be entered to populate the <City> and <State> fields.
4.2 Modify PATIENT_INSURANCE screen
4.2.1 If currently setup with Medi-Cal insurance as ‘P1 Primary 1’ (for non-CHDP visits) and CHDP as ‘P2 Primary 2’ (alternate primary), enter 06/30/2017 in the <Coverage To> field on the ‘P2 Primary 2’ insurance screen for CHDP. Please note:
• You are able to bill/rebill dates of service prior 7/1/2017 to the CHDP insurance.
• All new charges are submitted to the Medi-Cal insurance.
4.2.2 If currently setup with CHDP insurance only as the ‘P1 Primary 1’ insurance:
• Enter 06/30/2017 in <Coverage To> field for CHDP insurance.
• Add new ‘P1 Primary 1’ insurance for Medi-Cal with <Coverage From> set to 07/01/2017.
What about the information on the PM160 that is not included on the national claim forms (CMS1500, UB04 or electronic equivalents)?
Although some of the fields on the PM160 are NOT REQUIRED on the national claim forms (and should not be included on the claims), it may still be required to document the information in the patient’s chart, perform assessments and immunizations at recommended intervals, or use specific procedure codes with modifiers to indicate partial screening services. These fields include:
• L.A. Code
• COUNTY CODE
• Next CHDP Exam
• HEIGHT
• WEIGHT
• BODY MASS INDEX (BMI)
• BLOOD PRESSURE
• HEMOGLOBIN
• HEMATOCRIT
• BIRTH WEIGHT
• Tobacco Use
Please refer to the resources available on the Medi-Cal website for specific program requirements.
Additional Resources from Medi-Cal website:
• CHDP Frequently Asked Questions
• CHDP Program Code Conversion Table
• CHDP Provider Manuals and Bulletins
• CHDP Code Conversion Readiness Checklist (5/12/2017)
• Reminder: Upcoming Changes to CHDP Billing (5/16/2017)