
Intellect™
BILLING MENU OPTIONS

Tele Com
Verify
Group of Patients
This menu option is used to electronically submit groups of scheduled patients to insurers to verify their eligibility. Since clinics are set for automation most of the time, this screen is most useful for manually submitting specific accounts.
For Tele Com verification, these conditions must exist:
• A patient must be on the schedule for the requested date range.
• An account must be set up with the Verification vendor.
• For the Verification vendor, the Utility --► Insurance --► Insurance <Eligibility> field must match the <Carrier Type> entered here.
• For the Verification vendor, the Utility --► Insurance --► Insurance <Eligibility Receiver> field must have the proper code.
• Utility --► Insurance --► Tele Com for the Verification vendor must be completed, with the <270 Script> field set according to the carriers' requirements.
• There must be an approved method of transmittal for the Verification vendor; e.g., modem or secure FTP or FT.
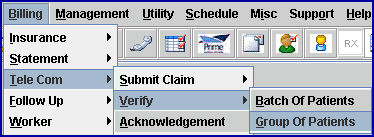
1. To submit a group of patients in Intellect, go to Billing --►Tele Com --► Verify --►Group of Patients
The Verify GOP Eligibility screen displays:
2.1 Type a beginning date for Intellect to search the Schedule.
3. Appointment To Date 
3.1 Type an ending date for Intellect to search the Schedule.
4.1 Enter the Utility --► Insurance --► Insurance <Electronic Billing> code for this carrier:
4.2 This field is required.
5. Insurance Code 
5.1 Type the Utility --► Insurance --► Tele Com <Insurance Code>.
5.2 This is required.
6. When the information is completely entered, select one of these options:
6.1 Click [Verify] to create a file and transmit it to the designated carrier.
6.2 Click [Clear] to clear all information and return the focus to the <Appointment From Date> field without saving.
6.3 Click [Exit] to clear the screen and return the focus to the main Intellect screen without saving.
The Verification Request (271) is picked-up through Billing --► Tele Com --► Acknowledgement <Status> = 'P.'
Once the file is picked-up, individual patient coverage records may be viewed in the Billing --► Tele Com --►Eligibility --► Modify screen.
Note: Eligibility responses vary from payer to payer. Some payer responses are very robust and include quite a bit of benefits information in addition to the eligibility response. Others are more limited in the information that they provide. If the information is not required in a 271 response, there is no way to make the payer send it. For example, Cognizant (formerly Trizetto) always returns all of the information to the office that they receive from each payer. Please remember that this is just an Eligibility verification. This tells the provider if the patient is eligible for services on the date submitted.