
Intellect™
BILLING MENU OPTIONS

Tele Com
Eligibility
Eligibility Modify
Updates:
Effective version 21.04.14
New Inovalon/Ability All Ease Payer integration for Eligibility Verification is now available.
Prime Clinical Systems developed another API solution for the Eligibility Verification for the Inovalon/Ability All Ease Payer Solution to function the same as the current method of OnStaff/Intellect Eligibility Verification. Contact PCS for details.
Announcement in version 18.03.14 release note:
Eligibility TLS/TPS Changes for Cognizant/TriZetto Clients
span style="font-family: Arial, sans-serif;">New requirements have been assigned by Cognizant/TriZetto for TLS in using the ELIGIBILITY features in the Intellect software. Cognizant stated, "In an effort to enhance our current product functionality and capabilities, we are in the process of upgrading your Master Eligibility Web Service (MES) offering. TPS will disable TLS 1.0 security protocol by end of year 2018, and is requesting clients upgrade their systems to accommodate TLS 1.1 and/or 1.2 protocols prior to this date." (emphasis added). In response to Cognizant's changes, Prime Clinical Systems has made the necessary changes to our software to comply with Cognizant/TriZetto's product. If an office uses Cognizant/TriZetto as their Clearing House Solution, the office requires an Intellect update to a version date greater than 2/28/2018. This change is seamless and requires no action on the part of the office once the software is updated. Failure to update to an Intellect version date greater than 2/28/2018 prior to December 2018 results in a non-functioning Eligibility feature within Intellect.
This menu option is used to display and maintain Insurance billing eligibility records for patients' accounts. When a client is set up for Tele Com electronic transactions using an approved Verification vendor, this screen populates with the Verification Request sent by Billing --►Tele Com --►Verify (270) and picked-up by Billing --►Tele Com --►Acknowledgement (271).
Also, specific patient accounts may be manually added via Billing --►Tele Com --► Eligibility --►Add.
For Tele Com Eligibility Verification, these conditions must exist:
• A patient must be on the schedule for the requested date range.
• The requested insurance(s) is listed as one of the patient's insurance screen(s).
• The patient's Utility --► Insurance --► Insurance <Eligibility> field must match the insurance entered here.
• The patient's Utility --► Insurance --► Insurance <Eligibility Receiver> must have the proper code.
• Utility --► Insurance --► Tele Com must be completed.
• An account must be set up with a receiving agency.
• There must be a carrier-approved method of transmittal: modem, secure FTP, or FTP.
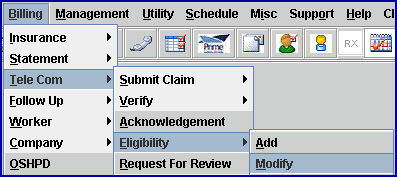
1. To modify or view eligibility in Intellect, go to Billing --►Tele Com --► Eligibility --►Modify
The Modify Eligibility screen displays:
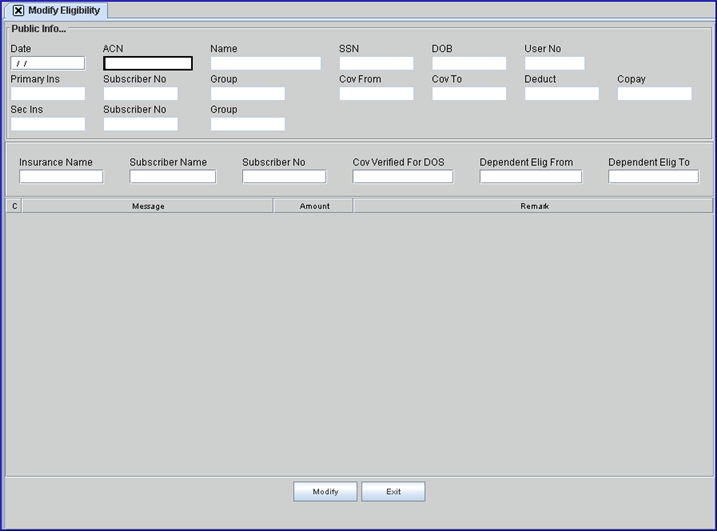
Once an 'Eligibility' record is added, it is keyed by a combination of the patient account number <ACN> and the date of verification <Date>. You must correctly match both field entries to modify/display a record.
2.1 Enter the date the patient verification was completed (e.g., date the 271 was picked-up).
2.2 When searching for an account to modify/display, when the date of verification (271) is not known the date field may be left blank. Press [F2] to display a Searching screen to search for available records.
2.2.1 When records are found where the date of verification(s) match the entered <ACN> (patient account number), search results are displayed. To select, double-click on the desired record, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct record, and then press the [Enter] key to select. For more information on the Searching feature, see Introduction to Intellect --► Intellect Characteristics and Features - Searching.
2.2.2 When Intellect is unable to find results for the entered <Date> and <ACN>, this message displays. Click [OK] to return to the Modify Eligibility screen.
3.1 Type the patient account number whose eligibility status is desired to view/modify.
3.2 If a record was selected from the [F2] date search above, this field populates.
After pressing [Enter], [Tab] , or ↓ (down) arrows, the screen fills-in and the focus moves to the <Insurance Name> field:
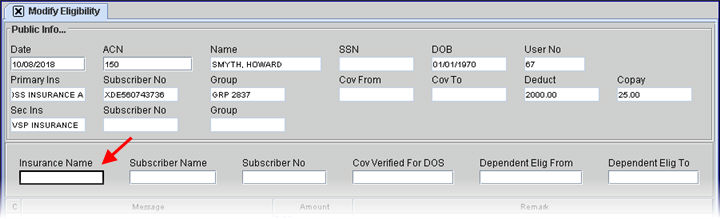
4. Name 
4.1 The associated name displays from the entered account number: Last, First.
4.2 This is a read-only field and may not be modified.
5. SSN 
5.1 The patient's social security number displays based on the <Social Security No> field on the Registration--► Regular --►Patient screen.
Effective version 16.12.02, the options of masking the SSN (displaying only the last 4 digits) or not masking the SSN are now available. For additional information, see Utility --►Set Up --►Screen Fields, Masking/Unmasking the Social Security Number (SSN).
Effective version 16.11.10, the SSN only displays the very last 4 digits and the rest are represented with asterisks (***-**-1234), unless the data in the database is malformed or incomplete.
5.2 This is a read-only field and may not be modified.
6. DOB 
6.1 The patient's date of birth displays based on the Registration --►Regular --►Patient <DOB> field.
6.2 This is a read-only field and may not be modified.
7. User No. 
7.1 Displays the Utility --►Set Up --►Security --►Log In Users <User Number> for the current operator.
7.2 This is a read-only field and may not be modified.
8. Primary Ins 
8.1 The primary insurance company name displays based on the Registration --►Regular --►Patient Insurance <Insurance Company Name> field.
8.2 This is a read-only field and may not be modified.
9. Subscriber No 
9.1 The subscriber number displays based on the Registration --►Regular --►Patient Insurance <Subscriber No> field for the primary insurer.
9.2 This is a read-only field and may not be modified.
10. Group 
10.1 The group number displays based on the Registration --►Regular --►Patient Insurance <Group No> field for the primary insurer.
10.2 This is a read-only field and may not be modified.
11. Cov From 
11.1 The coverage begin date displays based on the Registration --►Regular --►Patient Insurance <Coverage From> field for the primary insurer.
11.2 This is a read-only field and may not be modified.
12. Cov To 
12.1 The coverage end date displays based on the Registration --►Regular --►Patient Insurance <Coverage To> field for the primary insurer.
12.2 This is a read-only field and may not be modified.
13. Deduct 
13.1 Intellect displays the <Deductible Met> info from the Registration --►Regular --►Patient Insurance screen.
13.2 This is a read-only field and may not be modified.
14. Copay 
14.1 Intellect displays the <Co Payment> info from the Registration --►Regular --►Patient Insurance screen.
14.2 This is a read-only field and may not be modified.
15. Sec Ins 
15.1 The secondary insurance company name displays based on the Registration --►Regular --►Patient Insurance <Insurance Company Name> field.
15.2 This is a read-only field and may not be modified.
16. Subscriber No 
16.1 The subscriber number displays based on the Registration --►Regular --►Patient Insurance <Subscriber No> field for the secondary insurer.
16.2 This is a read-only field and may not be modified.
17. Group 
17.1 The group number displays based on the Registration --►Regular --►Patient Insurance <Group No> field for the secondary insurer.
17.2 This is a read-only field and may not be modified.
Press [Enter], [Tab] , or ↓ (down) arrows through the remaining fields to move to the Command Column.
18. Insurance Name 
18.1 The payer's name for the requested insurer.
19. Subscriber Name 
19.1 The payer's name for this subscriber.
20. Subscriber No 
20.1 The subscriber number for this patient for this payer.
21. Cov Verified For DOS 
21.1 The patient’s scheduled date verification.
2. Dependent Elig From 
22.1 Enter the date the dependent became eligible.
23. Dependent Elig To 
23.1 Enter the date the eligibility of the dependent ends.
After pressing the [Enter], [Tab] , or ↓ (down) arrows, the focus moves to the Command Column:
24. C (Command Column) 
24.1 With the focus in the Command Column, press [F2] to see the valid choices:
24.2 The <Amount> and the <Remark> columns may be modified.
25. Message 
25.1 Displays the line item description from the payer. This field is always blank for user-added verifications.
Note: Prior to version 9.12.13, Response Code AAA67, used by the insurance when the patient was not found in their eligibility records, was not programmed in Intellect. Therefore, nothing would show in Intellect's Eligibility History. Effective version 9.12.13, the 271 Response Code AAA67 was added to the eligibility verification programming, allowing the code to be inserted into the patient's Intellect eligibility record and the description to be displayed in the patient eligibility history.
26.1 Displays the line item description.
26.2 This column may be modified.
27.1 Displays the line item clarification or notation.
Note: Prior to version 9.12.13, Response Code AAA67, used by the insurance when the patient was not found in their eligibility records, was not programmed in Intellect. Therefore, nothing would show in Intellect's Eligibility History. Effective version 9.12.13, the 271 Response Code AAA67 was added to the eligibility verification programming, allowing the code to be inserted into the patient's Intellect eligibility record and the description to be displayed in the patient eligibility history.
27.2 This column may be modified.
28. When the information is completely entered, select one of the options:
28.1 Click [Modify] to commit any changes and clear the screen, returning the focus to the <Date> field.
28.2 Click [Exit] to exit without saving, returning to the main Intellect screen.
View Sample Data From 271 File