
Intellect™
BILLING MENU OPTIONS

Insurance
Batch of Patients
This menu option is used to print an individual claim or a small batch of Insurance claims for patients’ accounts.
NOTE: The ‘Pre-Billing Report’ may only be run using Billing --► Insurance --► Group of Patients.
Very often a client's billing is set for automation; therefore, this screen is most useful for printing specific claims.
Note: When a patient changes insurance, the old insurance information should be left in the patient's demographic screens until all charges/payments have been completed for the old carrier. If the old insurance is removed prior to completion of charges/payments, Intellect does not generate the information for the old insurance on the statements.
For billing and rebilling, these conditions must exist:
• A charge/date of service exists within the requested date range.
• The requested insurance(s) is listed as one of the patient's insurance screen(s).
• The date(s) of service must fall within the patient's insurance screen's <Coverage From> and <Coverage To> date range.
See details for opening and populating the Print BOP Insurance screen.
Updates:
Effective version 21.11.09: In previous releases, the treating provider was added to Box 77 of the UB04 form. However, this box was only to be used when there was a surgical procedure being done and the assistant surgeon needed to be listed on the claim.
The new changes now omit the information from Box 77 when the Utility --► Procedure <POS> is Surgical and the conditions are met in Report Designer. If at the time the user adds a referring provider to the charges, the referring providers name and information are printed in this box.
Effective Version 9.12.34
The 'B' option added in version 9.12.30 (see entry below) to the drop-down menu of the <Billing Sorting> field on the Utility --►Set Up --►Parameter screen was removed.
The function of the 'B' option is now performed by the 'Batch' option on the new <Batch Sorting> field added to the Utility --►Set Up --►Parameter screen. The 'Batch' option sorts the batch in the order the accounts were entered into the Batch Entry screen.
The system uses the <Batch Sorting> field to sort the results when printing a report, or from Batch of Patient screens in Billing--►Insurance, Billing --►Statement, Billing --►Worker --►Statement, Billing --►Worker --►HCFA forms, and Billing --►Worker --►Attorney.
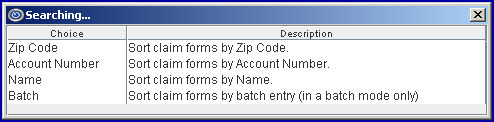
The sort options are:
A new 'B' option was added to the drop-down menu of the <Billing Sorting> field on the Utility --►Set Up --►Parameter screen:
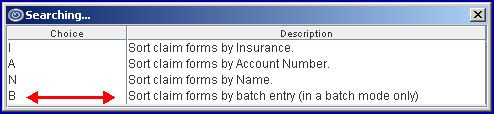
As shown in the Description above, option 'B' is used only for Batch of Patient tasks.
• If option 'B' is selected when running tasks using Batch of Patients, the billing is in the order the account numbers were entered on the Billing --►Insurance --►Batch of Patients screen.
• If option 'B' is selected when running tasks using GOP, it is as if option 'A' had been selected in the <Billing Sorting> field since the results are ordered by Account Number.
This change affects Billing --► Insurance, Billing --►Worker --►Statement, Billing --► Worker --► HCFA Form, and Billing --►TeleCom --►Submit Claims.
The new option does not affect Billing --►Statement, Billing --►Worker --►Letter, Billing --►Worker Attorney, or Billing --►Company Statement.
Effective version 9.12.14
Users have the option to select which insurances should be billed for zero balances and which should not when they are the patient's secondary or tertiary insurance. To facilitate this change, a <Bill Zero Balance> field was added to the Utility --►Insurance --►Insurance screen (this field is for paper billing only). Please refer to Utility --►Insurance --►Insurance <Bill Zero Balance> for set up information.
Prior to version 9.12.14, if when the primary payment and adjustment are posted the balance was zero and the patient has secondary insurance, the program would bill the secondary insurance unless the Who column was modified to G before billing was run.
Video Available: Click Billing Insurance Form to access the links. Depending on the system set up, the media player may need to be activated. Speakers need to be attached to the workstation to hear the instructions.
Note: To view the videos, log-in through the www.primeclinical.com website. Current support is required.
1. To open the Print BOP Insurance screen in Intellect, go to Billing --► Insurance --► Batch of Patients
The Print BOP Insurance screen displays:
Effective Version 9.12.10 - Field Modification. The one- and two-character code choices on the drop-down lists have been replaced with explanatory choices, making the code selection more user-friendly and comprehensive.
Note: The drop-down list descriptions for the code choices have remained the same, allowing correlation between the old and new code choices.
2. Account No 
2.1 Type the patient account number whose insurance to bill.
2.2 Press [Enter] to open the Batch Entry dialog screen to allow more accounts to be individually added to process as a single batch.
2.3 Type any additional account numbers (one at a time) and press [Enter] to add.
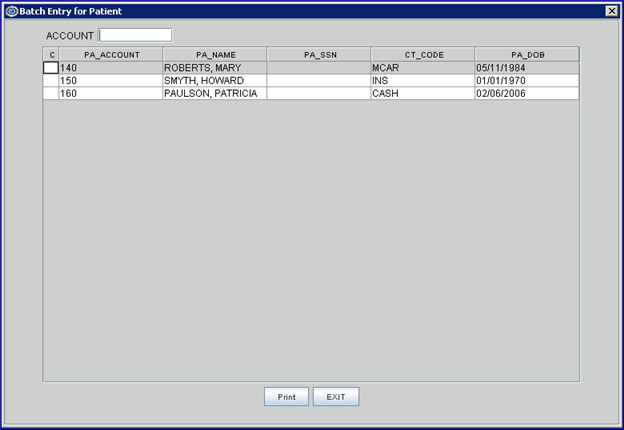
2.4 Click [Print] to reserve the information for the accounts entered and return to the <From Date> field on the Print BOP Insurance screen
2.5 Click [Exit] to return to the <From Date> field on the Print BOP Insurance screen and clear the Batch Entry for Patient screen.
3. From Date 
3.1 Enter the beginning date of the date range for charges to be billed/rebilled based on the <Date Selection (E/S/P/B)> field criteria.
3.2 If left blank, Intellect defaults the calendar date.
4. To Date 
4.1 Enter the last date of the date range for charges to be billed/rebilled based on the <Date Selection (E/S/P/B)> field criteria.
4.2 If left blank, Intellect defaults the calendar date.
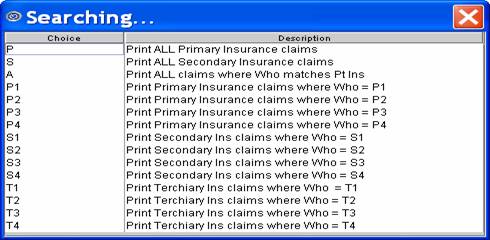
5.1 Use this to select which insurance bill to print.
5.2 Accept the 'P All Primary Insurances' default (formerly P) for this group of patients, OR use the drop-down list to make an alternate selection.
5.3 Click on the field, OR press the [F2] key to display the valid choices.
To view the list of only the codes, click on the arrow. To select, click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code and then press the [Enter] key to select.
Effective version 9.12.10
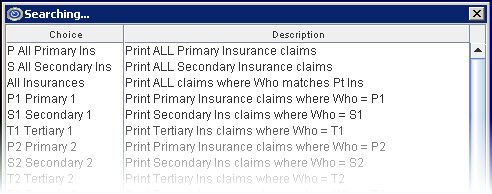
All versions prior to 9.12.10
6. All/Unbill/Rebill/(A/U/R/H) 
6.1 This is a selection field to determine which status of claims to print.
6.2 Accept the 'Unbilled Charges' default (formerly U), OR use the drop-down list to make an alternate selection.
6.3 Click on the field, OR press the [F2] key to display the valid choices.
To view the list of only the codes, click on the arrow. To select, click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code and then press the [Enter] key to select.
Effective version 9.12.10
NOTE: Use option Multiple Insurances (formerly M) only for Workers Compensation claims.
All versions prior to 9.12.10
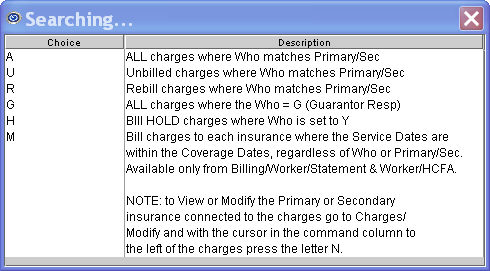
6.4 Effective version 16.12.02 the 'Multiple Insurance' drop-down option now allows users to print the HCFA 1500 for charges to each patient insurance.
7. Category 
7.1 This field limits the billing results by specific patient category.
7.2 Press [Enter] to bypass this field, which requests ALL categories, OR use a specific category by typing its Utility --► Category <Category Code>.
7.3 This field accepts multiple values:
• Category codes separated by commas with no spaces:
• a range of codes entered with a hyphen and no spaces:
• an asterisk * to return all Categories starting with the portion of the code entered prior to the *. For example, M* prints all Categories whose code begins with M.
7.4 Effective version 14.11.19: When the Utility --►Insurance --►Insurance <Insurance Type> field is set to 'B', paper billing for Worker's Comp patients now prints the Utility --►Provider --►Provider <Taxonomy> field in Box 24J above the <NPI>.
Note: When printing the HCFA from Billing --►Insurance, this <Category> field must be set to a Worker Category.
ATTENTION: This IMMEDIATELY affects billing and other daily tasks.
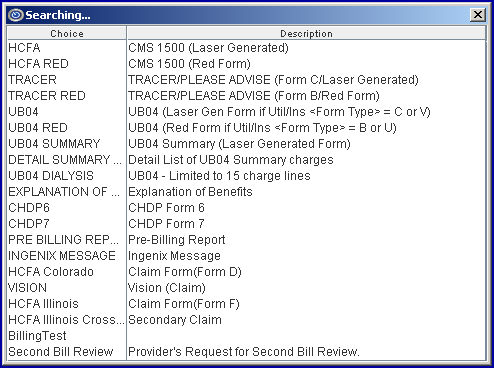
8.1 Accept the default 'HCFA', OR use the drop-down list for an alternate selection. See form samples.
Please note:
8.1.1 NOTE 1: Version 14.03.20 or higher is required to use HCFA 1500 Form (02-12) mandated for use beginning April 1, 2014.
• For black and white forms, select NEW HCFA
• For the red and white forms, select NEW HCFA RED
8.1.2 NOTE 2: Claims only print when this <Form Type> selection matches the Utility --► Insurance <Form Type>.
8.1.3 The Pre-Billing Report option (formerly P) is ONLY available from Billing --► Insurance --► Group of Patients.
8.1.4 When the 'Ingenix Message' option is selected, the same information is gathered as for billing reports, only it is saved in a special format, like HL7. The file name begins with IMF, and is saved under ut_path/ingenix.
8.1.5 Effective version 16.10.11, the drop-down options of CHDP 6 and CHDP 7 were removed. An option of CHDP was added to accommodate the most current version (CHDP 8, at the time of the update).
8.1.6 The EXPLANATION OF BENEFITS option only prints if the <Who> field for the requested charges is set to ‘S1’ (or an alternate secondary insurance ‘S2’, ‘S3’, etc.).
8.1.7 Effective version 23.10.04: When the Utility --►Insurance <Insurance Type> is D (Medi-Cal) and Billing --► Insurance <Form Type> is NEW HCFA RED, Box 3 (DOB) prints as a 6-digit date (MM/DD/YY) as required by Medi-Cal (see CMS-1500 Completion, Item 3).
8.2 Click on the field, OR press the [F2] key to display the valid choices.
To view the list of only the codes, click on the arrow. To select, click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code and then press the [Enter] key to select.
Sample code lists are shown below for these versions:
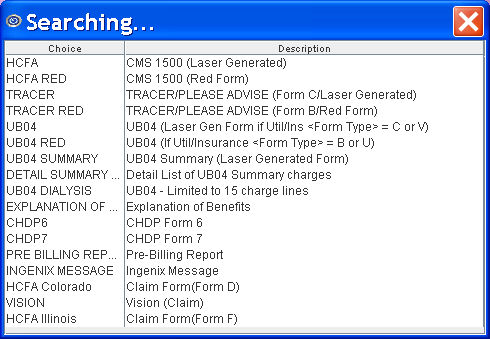
In the 9.12.10 update, some unused codes were removed from this list.
Version 9.12.14 - Modification. In this update, the headings for the Pre-Billing report were split into two lines. Additionally, Ref Prv was added under Pt Name, Tx Prv was added under Submitter#, and Bl Prv was added under Group#.
NOTE: In order to accommodate Medi-Cal billing restrictions for Dialysis claims on UB-04, which limit charge lines to 15 instead of the usual 22, Form Type UB04 Dialysis (formerly 'A') may be selected. The Utility --► Insurance screen does not require any change.
In the13.06.24 update, the Second Bill Review option was added. The Second Bill Review option works in conjunction with Payment --►Open Item in requesting that a DWC Second Bill Review (SBR) form be printed for submitting a Worker's Compensation payment appeal. In Payment --►Open Item, see set up information for the Message and Comment columns.
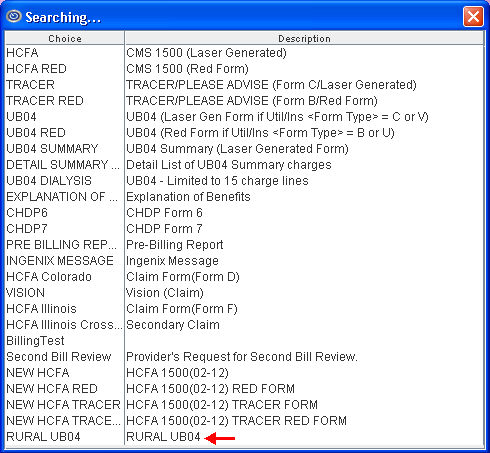
Version 13.12.12: A RURAL UB04 report was added for clients using Managed Care. This report is similar to UB04 SUMMARY, and works with the Utility --►Insurance --►Insurance <Form Type> options C and 8, the same as the UB04 Summary report. As a result, clients that used to print the UB04 Summary do not need to change their insurance screen settings for the new RURAL UB04 report.
The RURAL UB04 report option differs from the UB04 Summary as follows:
Box 18 always prints "80"
Box 42 is blank
Box 43 prints "Managed care diff rate"
Box 44 prints "18"
Box 50, when billing S or T insurances, only prints the address to insurance information
Box 58 through Box 62 are Blank
Version 16.02.22: A Dispute Resolution Request form was added for use by the office to dispute payments or underpayments. When generating the form, Intellect pulls the insurance attached to the patient record, the provider name and address, the provider tax id number, the patient name and date of birth, and the patient subscriber ID.
The amounts that print on the form are based on the provider for whom the form is printed/generated, the From and To dates of service, and the total billed. If the form needs to be generated for more than one provider, each provider must be requested separately in the <Provider> field.
Before a dispute resolution form may be requested:
• Each provider for whom a dispute resolution form is generated must have his/her own PDR code set up in <Message Code> on the Utility --►Messages --►Message screen.
• The appropriate PDR code must be added in the Message column on either the Payment --►Open Item screen or the Ledger --►Open Item screen for the charge/payment in dispute.
9.1 This field limits the billing results by specific patient insurance companies.
9.2 Press [Enter] to bypass this field, which requests ALL insurance companies, OR select a specific insurance by typing its Utility --►Insurance --►Insurance <Insurance Co. Code>.
9.3 This field accepts multiple values:
• Insurance codes separated by commas with no spaces:
• a range of codes entered with a hyphen and no spaces:
• an asterisk * to return all Insurers starting with the portion of the code entered prior to the *. For example, B* prints all Insurers whose code begins with M.
10. Billing Code 
10.1 For use with <All/Unbill/Rebill (A/U/R/H)> = 'R' Rebill.
10.2 The default is to submit billing for all billing codes (leave blank).
10.3 To filter the billing based on specific billing codes, type the Ledger --►Open Item <Message>.
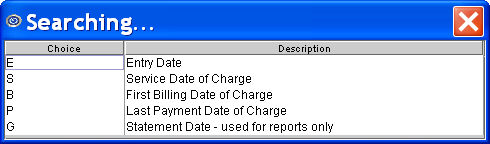
11.1 This field defaults to the Entry Date.
11.2 Accept the default OR use the drop-down list to make an alternate selection.
11.3 Click on the field, or press the [F2] key to display the valid choices.
To view the list of only the codes, click on the arrow. To select, click on the correct code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code and then press the [Enter] key to select.
Effective version 9.12.10
All versions prior to 9.12.10
12.1 The default (blank) submits billing for all providers.
12.2 To filter the billing based on a specific provider, type the Utility --► Provider <Provider Code>.
12.3 This field accepts multiple values:
• provider codes separated by commas with no spaces:
• a range of codes entered with a hyphen and no spaces:
• an asterisk * to return all Providers starting with the portion of the code entered prior to the *. For example, 2* prints all Providers whose code begins with 2.
13. User# 
13.1 The default (blank) submits billing for all users (operators).
13.2 To filter the billing based on a specific user, type the Utility --► Set Up --► Security --► Login Users <User Number>.
14.1 The default (blank) submits billing for all POS.
14.2 To filter the billing based on a specific POS, type the Utility --► Facility <Facility Code>.
14.3 This field accepts multiple values:
• facility codes separated by commas with no spaces:
• a range of codes entered with a hyphen and no spaces:
• an asterisk * to return all facilities starting with the portion of the code entered prior to the *. For example, 1* prints all facilities whose code begins with 1.
14.4 Effective version 21.11.09, changes were made when a surgical facility is entered in this field. See the Updates section at the beginning of this document for details.
15. Department 
15.1 The default (blank) submits billing for all Provider Department Numbers.
15.2 To filter the billing based on a specific Department, type the Utility --► Provider --► Provider <Department> name or number.
15.3 This field accepts multiple values:
• departments separated by commas with no spaces:
• a range of codes entered with a hyphen and no spaces:
• an asterisk * to return all facilities starting with the portion of the code entered prior to the *. For example, 1* prints all facilities whose code begins with 1.
16. When the information is completely entered, select one of these options:
16.1 Select the [Print] button OR press [Enter] to display the printer dialog box:
16.1.1 Printer Properties:
16.1.1.1 Printer: The default printer for the logged-in clinic and password is selected. To select a different printer, either click on the arrow, OR press the → (right arrow) on the keyboard to view the list of printer codes. In our example, the defaulted Printer is HP. This is just an example of a printer name and may or may not be set up on the system.
Select the printer type by clicking on the code, OR use the ↑ (up) and ↓ (down) arrows to highlight the correct code, and then press the [Enter] key to select.
16.1.1.2 Number of Copies: This field defaults to either 0 (zero) or 1. Both print 1 copy. To print more than one copy, enter the number of copies.
16.1.2 Fax/Email:
In addition to printing reports, Intellect provides the capability to export reports to Email, Fax, Disk, or Archive. A secondary printer may also be selected, if one is set up, by clicking on the arrow to display the drop down list.
16.1.3 Select the [Print] button to send the request to the printer (or as a Fax or email). NOTE: After printing claim forms, the remark ‘BILL WAS SENT TO THE INSURANCE’ From: [date of service] To: [date of service]’ with <Flag> set to ‘I’ is automatically added to the Ledger remarks on both the Ledger --► Accounting --► Display and Ledger --► Open Item --► Display screens for each patient if Utility --► Set Up --► Parameter <Message (Y/N)> is set to ‘Y.’
16.1.4 Select the [Cancel] button to clear the screen and return to the <Account No> field without saving or printing.
16.2 Click [Clear] to clear all information and return the focus to <Account No> field without saving.
16.3 Click [Exit] to clear the screen and return the focus to the main Intellect screen without saving.