
Intellect™
BILLING MENU OPTIONS

Quick Resources
CMS 1500 Box Definitions
and
BILLING MENU OPTIONS

Worker
HCFA Form
CMS 1500 Box Definitions
Please use this as a guide to complete billing forms accurately. Each box of the CMS 1500 claim form is reviewed. Noted per box is the exact Intellect location of the printed information and billing method criteria when applicable.
Effective Version 14.07.01
Per this version, there were three modifications:
• Intellect now prints 6 lines instead of 5 lines of service on the HCFA 1500 Form.
• When billing an insurance with the Utility --►Insurance --►Insurance <Insurance Type> field set to either D or 1 (Medi-Cal or Medi-Medi), HCFA Box 30 now displays the Balance Due based on the Utility --►Insurance --►Insurance <Include Payment> field setting. This modification affects NEW HCFA and NEW HCFA RED and Tracers. To use this option, please notify a PCS Support team member.
• Boxes 4, 7, and 9 now print blank (instead of 'SAME') when the insured is the same as the patient.
Box 1 MEDICARE, MEDICAID, CHAMPUS, CHAMPVA, GROUP HEALTH PLAN, FECA BLK LUNG, OTHER
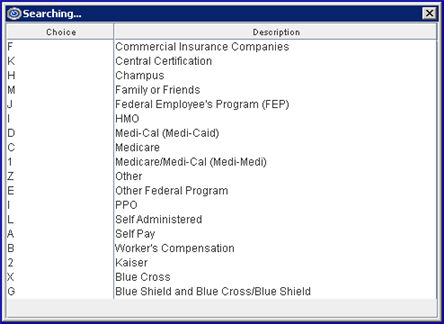
The box is checked based on the type of insurance entered in the Utility --►Insurance --►Insurance <Insurance Type> field. With the cursor on this field, press [F2] to display this list:
*837 Electronic Claims Submission Equivalent Loop 2000B SBR09
This prints the insurance I.D. from the Registration --►Regular --►Patient Insurance screen <Subscriber No.> field.
*837 Electronic Claims Submission Equivalent Loop 2010BA NM109
Box 2 PATIENT'S NAME
This prints the patient name from the Registration --►Regular --►Patient <Last Name>, <First Name>, <Middle Initial> fields.
*837 Electronic Claims Submission Equivalent Loop 2010BA NM 103,04,05,07
This prints the birth date of the patient from the Registration --►Regular --►Patient <DOB> field.
*837 Electronic Claims Submission Equivalent Loop 2010BA DMG02
If the patient is a dependent OR a secondary claim form is being printed AND other than self is the insured, then the name of the insured prints from the Registration --►Regular --►Patient Insurance screen <Last Name>, <Insured First Name>, <Middle Initial> fields.
If the patient is the insured when billing Medicare as their secondary coverage, then 'SAME' prints here.
Note: Effective Version 14.07.01, this field prints blank (instead of 'SAME') when the insured is the same as the patient.
For Workers Compensation patients (Utility --►Category <Type> = W) Registration --► Worker --► Worker Insurance <Employer> is used.
*837 Electronic Claims Submission Equivalent Loop 2010BA NM 103,04,05,07
Box 5 PATIENT'S ADDRESS, CITY, STATE, ZIP CODE, TELEPHONE
The full address and phone number of the patient prints from the Registration --►Regular --►Patient <Address>, <Zip Code>, <City>, <State>, and <Home Phone No> fields.
*837 Electronic Claims Submission Equivalent Loop 2010BA NM 301,02
The appropriate box is checked based on the information entered on the Registration --►Regular --►Patient Insurance screen <Relation to Insured> field. Valid field entries are:
18 - Self
1 - Spouse
19 - Child
- Other
*837 Electronic Claims Submission Equivalent Loop 200B SBR02 PAT01
Effective version 9.12.28, for Worker HCFAs, when the client is registered under the Worker menu, the system populates Box 6 with 'Other,' by default.
Note: This change is not automatically added with the 9.12.28 update. To have this change, call Prime Clinical Systems and request the HCFA form be updated.
If the patient is a dependent OR a secondary claim form is being printed, then the address of the insured prints from the Registration --►Regular --►Patient Insurance <Address>, <Zip Code>, <City>, <State>, and <Home Phone No> fields.
If the patient is the insured when billing Medicare as their secondary coverage, then 'SAME' prints here. Note: Effective Version 14.07.01, this field prints blank (instead of 'SAME') when the insured is the same as the patient.
For Workers Compensation patients (Utility --►Category <Type> = W) Registration --► Worker --► Worker Insurance <Address>, <Zip Code>, <City>, <State>, and <Phone> fields are used.
*837 Electronic Claims Submission Equivalent Loop 2010BA N301,02
MARITAL:
This marks the appropriate marital status box according to the entry in the Registration --►Regular --►Patient (or Worker ) <Marital Status>. Valid selections are:
S: the 'Single' box is marked
M: the 'Married' box is marked
D: the 'Other' box is marked
EMPLOYED:
The employed box is marked according to the selection in the Charges --► Encounter --► Generic Encounter <Status: Employment> field when that encounter is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify.
FULL-TIME/PART-TIME STUDENT:
This marks the student status boxes according to the entry in the Charges --► Encounter --► Generic Encounter <Student (F/P/N)> field from the patients Encounter screen when that encounter is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify. Valid selections are:
F: the 'Full-Time Student' box is marked.
P: the 'Part-Time Student' box is marked.
If there is not an entry in this field, then the boxes are left blank.
When billing the primary, if the patient is the insured for the secondary coverage, 'SAME' prints here.
Note: Effective Version 14.07.01, this field prints blank (instead of 'SAME') when the insured is the same as the patient.
If the patient is a dependent, Intellect prints the Insured's name from <Last Name>, <Insured First Name>, <Middle Initial> fields from the Registration --►Regular --►Patient Insurance screen.
*837 Electronic Claims Submission Equivalent Loop 2330A NM 103,04,05,07
.
If the patient is a Medi-Medi patient (Medicare primary and Medi-Cal/Medicaid secondary) Intellect prints the ID obtained from the Registration --►Regular --►Patient Insurance <Group No.> field of the patients Medi-Medi insurance coverage screen.
All other cases with secondary coverage print 'MG' for Medigap plans plus the value found in the Registration --►Regular --►Patient Insurance screen <Subscriber No.> field.
*837 Electronic Claims Submission Equivalent Loop 2320 SBR03 /2330A REF02
If the patient is the insured, the date of birth and gender prints from the Registration --►Regular --►Patient <DOB> and <Gender> fields.
If the patient is a dependent, the date of birth and gender of the insured prints from the Registration --►Regular --►Patient Insurance <Insured DOB> and <Gender> fields.
*837 Electronic Claims Submission Equivalent Loop 2320 DMB02 and 2320 DMG03
If the patient is a dependent on the secondary coverage, the name of the employer prints from the Registration --►Regular --►Patient Insurance screen <Employer Name> field.
If the insurance coverage is secondary to Medicare, the name of the secondary insurance prints here from the Utility --►Insurance--►Insurance <Name>.
Use Utility --►Insurance --►Insurance <COBA> 5-digit ID for automatic crossover.
*837 Electronic Claims Submission Equivalent Loop 2320 SBR04/2320 NM103
a: EMPLOYMENT (CURRENT OR PREVIOUS)
The YES or NO box is marked according to the entry in the Charges --► Encounter --► Generic Encounter <Employment (Y/N)> when that encounter number is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify.
This marks the YES box only if an A is entered in the Charges --► Encounter --► Generic Encounter <Related Accident (A/O/N)> field. It also enters the patient’s state of residence.
If this field is blank or contains a value other than A, the NO box is marked.
c: OTHER ACCIDENT
This marks the YES box only if an O (alpha O) is entered in the Charges --► Encounter --► Generic Encounter <Related Accident (A/O/N)> field when that encounter number is associated with the charges being printed (the <EN#> field of Charges --►Charge OR Charges --►Modify). If this field is blank or contains a value other than O, the NO box is marked.
*837 Electronic Claims Submission Equivalent Loop 2300 CLM11 EM, CLM11 AA, CLM11 OA, CLM11, CLM11 AP
This should print MCD for Medigap crossovers.
If Medi-Cal is primary (Utility --►Insurance--►Insurance <Insurance Type> = D), and Charges --► Encounter --► Generic Encounter <Share of Cost Amount> has an entry, it prints here.
Effective version 9.12.28, for Worker HCFAs, Worker's Comp appeal codes were added to the drop-down menu in the <Report Type Code> field.
Note: This change is not automatically added with the 9.12.28 update. To have this change, call Prime Clinical Systems and request the HCFA form be updated.
If the Medicare or Medi-Cal (Medicaid) is primary (Utility --►Insurance--►Insurance <Insurance Type> = C or D), the word 'NONE' prints here.
If there is Insurance primary to Medicare, the Registration --►Regular --►Patient Insurance <Group No.> field prints here.
If the patient has a workers comp category type (Utility --►Category <Type> = W or F) the field is left blank.
All other cases with secondary coverage the value entered on the patient's Registration --►Regular --►Patient Insurance <Group No.> field prints here.
Note: For a CMS-1500 paper claim to be considered for Medicare Secondary Payer benefits, a copy of the primary payer's explanation of benefits (EOB) notice must be forwarded along with the claim form.
*837 Electronic Claims Submission Equivalent Loop 2000B SBR 03
Effective version 9.12.28, for Worker HCFAs, this box pulls the policy name.
In prior software versions, this box used to pull the name of the insurance company, as set up in Registration --►Worker --►Worker Insurance.
Note: This change is not automatically added with the 9.12.28 update. To have this change, call Prime Clinical Systems and request the HCFA form be updated.
If Registration --►Regular --►Patient Insurance <Relation to Insured> not = 18, the patient's date of birth and gender from the patient's Registration --►Regular --►Patient <DOB> and <Gender> fields prints here.
*837 Electronic Claims Submission Equivalent Loop 2010BA DMG02 and DMG03
When billing secondary, if Medicare is entered as the secondary coverage or if there is Medigap coverage in addition to Medi-Medi coverage, the entry from the patient's Registration --►Regular --►Patient <Employer Name> field prints here.
All other cases when billing secondary, Intellect prints the entry from the patient's Registration --►Regular --►Patient Insurance screen <Employer Name> field.
If Medicare (Utility --►Insurance --►Insurance <Insurance Type> = C) is entered as the secondary coverage, the name entered at Utility --►Insurance --►Insurance <Name> prints here.
If Medi-Medi (Utility --►Insurance --►Insurance <Insurance Type> = 1) is entered as the secondary coverage, the name entered at Utility --►Insurance --►Insurance <Payer Identifier> prints here.
All other cases with secondary coverage prints the Registration --►Regular --►Patient Insurance screen <Claim No.> field entry when its' Utility --►Insurance --►Insurance <Insurance Type> does not equal C.
*837 Electronic Claims Submission Equivalent Loop 2000B SBR 04
Effective version 9.12.28, for Worker HCFAs, this box is blank. In prior software, this box used to pull the policy name.
Note: This change is not automatically added with the 9.12.28 update. To have this change, call Prime Clinical Systems and request the HCFA form be updated.
For all insurance with secondary, the YES box is marked.
MEDICARE DOES NOT REQUIRE AN ENTRY
*837 Electronic Claims Submission Equivalent Loop
SIGNED: The patient's Utility --►Insurance --►Insurance <Message Box 12 & 13> field entry prints here.
DATE: Utility --►Set Up --►Clinic <Current Entry Date> prints here.
*837 Electronic Claims Submission Equivalent Loop 2300 CLM09 O106
Box 13 INSURED'S OR AUTHORIZED PERSON’S SIGNATURE
The patient's Utility --►Insurance --►Insurance <Message Box 12 & 13> field entry prints here.
*837 Electronic Claims Submission Equivalent Loop 2300 CLM08 2320 O103 CLM10 2320 O104
If the patient has a Worker's Comp category (Utility --► Category <Type> = W or F), this information prints from the Charges --► Encounter --► Generic Encounter <Injury Date> field when that encounter number is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify.
For all other category types, this information prints from the patient's Charges --► Encounter --► Generic Encounter <First Symptom> field when that encounter number is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify.
*837 Electronic Claims Submission Equivalent Loop 2300 DTP03
This information prints from the patient's Charges --► Encounter --► Generic Encounter <First Consulted> field when that encounter number is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify.
*837 Electronic Claims Submission Equivalent Loop 2300 DTP03
This information prints from the patient's Charges --► Encounter --► Generic Encounter <Disability From> and <Disability To> fields when that encounter number is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify.
*837 Electronic Claims Submission Equivalent Loop 2300 DTP03
For All Options below: If the referral source entered is not a physician (Utility --►Referring <Doctor/Other (D/O)> = O), Intellect prints the treating physician's name from the Utility --►Provider <Last Name> and <First Name> fields when the Utility --►Insurance --►Insurance <Insurance Type> is not D, F, or 5.
The name of the referral source (Utility --►Referring <Last Name> and <First Name> fields) prints here dependent on the Utility --►Set Up --►Parameter <Referring> field setting. Valid choices and where the printed information pulls from are:
P: Uses the <Referring Name> (a.k.a. ordering physician) from the patient file.
C: Uses the referring provider (a.k.a. ordering physician) entered at the time of posting charges (Charges --►Charge <Ref Prv>.
F: Looks first to the referral entered at the time of posting charges (Charges --►Charge <Ref Prv>). If no referring doctor (a.k.a. ordering physician) was entered at the time of posting charges, it looks to the patient file.
*837 Electronic Claims Submission Equivalent Loop 2310A NM 103,04,05,07
Software releases affecting Box 17 include:
Version 15.09.28 Printing the Ordering Provider on HCFA's
Version 14.11.19 Medicare Paper Claims
Version 14.08.25 DME Billing
Version 14.07.01 General Billing
Following the above criteria for Box 17:
17a prints the associated identification number as requested in Utility --► Insurance --► Insurance <Box 17a> from either Utility --►Referring or Utility --►Provider.
For proper billing, the selection in Utility --► Insurance --► Insurance <Box 17a> should match Utility --► Insurance --► Insurance <Referring Type> which provides the qualifier for 17a
Following the above criteria for Box 17:
17b prints either Utility --►Referring <NPI> or Utility --►Provider --►Provider <NPI>.
*837 Electronic Claims Submission Equivalent Loop 2310A NM109
This prints the Charges --► Encounter --► Generic Encounter <Hospitalization From> and <Hospitalization To> when that encounter number is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify.
*837 Electronic Claims Submission Equivalent Loop 2300 DTP03
This prints from the Charges --► Encounter --► Generic Encounter <Box 19 Claim Notes> appended by <HCFA Box 19 Date> when the encounter number is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify.
Version 9.12.1 - New Option
Due to changes to the MediCal Anesthesia billing requirements for Box 19, effective by MediCal November 1, 2009, it is no longer necessary to print the Anesthesia Start and Stop times, and Total time. This change was added to Intellect in version 9.12.1. Note: For prior Intellect software versions, the 'Start Time', 'End Time', and 'Total Time' in military units prints for Anesthesiology billing when Utility --►Insurance --►Insurance <Insurance Type> = D (Medi-Cal/Medicaid).
Effective version 9.12.28, for Worker HCFAs, this box no longer pulls the Worker's Comp Specialty Code. Instead, since it is now required to add notes, the software now pulls the comments entered into the <Box 19 Claim Notes> field.
Note: This change is not automatically added with the 9.12.28 update. To have this change, call Prime Clinical Systems and request the HCFA form be updated.
If Utility --►Procedure <Status> = 'L' lab
And if Charges --► Encounter --► Generic Encounter <Referred Lab> is configured with a facility code, then Intellect places an 'X' in the Yes Box of Outside Lab and, under the $CHARGES heading, prints the total cost for all charges where the Utility --►Procedure <Cost> field has an entry.
If posting charges without Charges --► Encounter --► Generic Encounter <Referred Lab> then, under the $CHARGES heading, it prints 'NO PURCH SVC'.
*837 Electronic Claims Submission Equivalent Loop 2300 AMT02
Note: When the Yes Box form Item 20 (Outside Lab) is checked, Item 32 of the claim form must be completed. When billing for purchased diagnostic tests, the provider of service must identify the supplier's name, address, zip code, and NPI in Item 32 of the claim form.
Note: The changes to HCFA forms are not automatically added with the update. to have these changes, call Prime Clinical Systems and request the form be updated.
In 21-1 through 21-4 based on the order entered at the time of posting (Charges --►Charge <Diagnosis Code>), this prints the ICD codes from the Utility --►Diagnosis <ICD10 Code> field for the dates of service(s) requested.
*837 Electronic Claims Submission Equivalent Loop 2300 HI01, HI02, HI03, HI04
Effective version 18.08.31: In software versions prior to 18.08.31, when a payment was received electronically and applied using the AutoPost feature, Intellect updated the charge history with the ICN # that came with the ERA file (this number is held in the background of the charges and is never visible to the user). This ICN# printed in Box 22 of the HCFA 1500 and was sent electronically. Due to recent requirements by payers to send corrected claims etc., and because the user does not have access to the ERA ICN#, a change was made in version 18.08.31 to print the ICN# (from the ERA) when the Charges --►Encounter screen has the <Claim Frequency Code> field set greater than 1, and the <Internal Control> field is blank.
This prints the Charges --► Encounter --► Generic Encounter <Medicare Status> code when the encounter number is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify.
Original Reference No
*837 Electronic Claims Submission Equivalent Loop 2300 REF02
Effective version 9.12.28, this change was made to Worker HCFAs:
Box 22a & b: This box is for replacement claims, corrected claims, or appealed claims. In other words, when a claim has been rejected and needs to be resubmitted. Section (a) of this box is filled with a 7 or 8, as entered into the <Claim Frequency Code> field. Section (b) of this box is filled with the Attachment Control Number from the pre-printed MEDI-CAL CLAIM Attachment Control Form, as entered in the <Identification Code> field. Note: The form must accompany the supporting documentation.
Note: This change is not automatically added with the 9.12.28 update. To have this change, call Prime Clinical Systems and request the HCFA form be updated.
If the patient has Medi-Cal (Medicaid) insurance coverage (Utility --►Insurance --►Insurance <Insurance Type> = D) this prints the Charges --►Encounter --►Generic Encounter <Authorization No.> entry when the encounter number is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify.
Box 23 pulls the Utility --► Provider <CLIA> number if these conditions are met:
• Utility --► Insurance <Print CLIA (Y/N)> = 'Y' for insurance being billed
• Utility --►Procedure <Status> = 'L' for the billed procedure.
If charges are linked to an encounter, the CLIA field entry from Charges --►Encounter --►Generic Encounter <Authorization No.> (see above) overrides entries made on this screen.
*837 Electronic Claims Submission Equivalent Loop 2300 REF02/2300REF02 (REF01=X4,G1,9F)
FROM: When entering charges (Charges --►Charge <From Date>), the entry prints as the FROM date.
TO : For all procedures whose Utility --►Procedure --►Procedure <Global (Y/N)> = N, when entering charges (Charges --► Charge <To>), Intellect enters a TO date that is equal to the FROM date.
For all procedures whose Utility --►Procedure --►Procedure <Global (Y/N)> = Y, when entering charges (Charges --► Charge <To>) is entered as the 'TO' date.
*837 Electronic Claims Submission Equivalent Loop 2400 DTP03
Based on the posted Charges --► Charge <Facility> code, Intellect pulls the Utility --► Facility <Place Of Service> code and prints it here.
*837 Electronic Claims Submission Equivalent Loop 2400 SV105
For all insurance types in Utility --►Insurance --►Insurance <Insurance Type>, this prints from the patient's Charges --►Encounter screen when the <Encounter #> field is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify unless the Charges --►Encounter <Emergency (Y/N)> field is null. If the <Emergency (Y/N)> field is null, the program pulls the Charges --►Encounter <Delay Reason Code> field and prints in 24C for Paper claims. BUT, if billing Electronic, the <Delay Reason Code> is not billed when the Charges --►Encounter <Emergency (Y/N)> is null.
*837 Electronic Claims Submission Equivalent Loop 2400 SV109
Based on the patient's assigned insurance Utility --►Insurance --►Insurance <Code (R/C/E/U)> field entry, the corresponding code from Utility --►Procedure --►Procedure <Code R>, <Code C>, <Code E>, <Revenue Code> and <Modifier R>, <Modifier C>, <Modifier E> (or modifier entered at the time of posting; i.e., Charges --►Charge <Code>) prints here.
*837 Electronic Claims Submission Equivalent Loop 2400 SV101
This prints the <RDX> field entry for charges being printed (Charges --► Charge OR Charges --►Modify). Medicare only accepts one related diagnosis per charge/procedure.
NOTE: For procedures with multiple Diagnosis pointers, the standard format is a space between: i.e., 1 2.
An optional format may be requested in which the space is eliminated; i.e., 12.
*837 Electronic Claims Submission Equivalent Loop 2400 SV107
This prints the amount from the posted Charges --► Charge <Charge>.
This amount is derived from Utility --►Procedure --►Procedure <Charge> field if a fee schedule has not been set up for the provider, insurance company, and panel code being requested (Utility --►Procedure --►Fee Schedule).
If a Utility --►Procedure --►Fee Schedule is set up for the provider, insurance company and panel codes are requested and the <Alt. Charge> amount is used.
*837 Electronic Claims Submission Equivalent Loop 2400 SV102
The value entered in the Utility --►Procedure --►Procedure <Days/Units> field prints here. If this value is modified at the time of posting, then the Charges --►Charge <Qty> entry prints.
*837 Electronic Claims Submission Equivalent Loop 2400 SV104
If the patient's insurance coverage is Medi-Cal (Medicaid) Utility --►Insurance --►Insurance <Insurance Type> = D this prints the selected code number from the patient’s Charges --►Encounter --►Generic Encounter <Family Planning> field when the encounter number is associated with the charges being printed from the <EN#> field of Charges --►Charge OR Charges --►Modify.
*837 Electronic Claims Submission Equivalent Loop 2400 SV111
Intellect uses the selection from Utility --►Insurance --►Insurance <Box 24J Type> to print the rendering provider’s legacy number qualifier for the ID as requested by this insurer.
*837 Electronic Claims Submission Equivalent Loop 2010AA REF01
Regardless of billing method, Intellect selects and bills based on the program’s hierarchy.
Intellect first looks in the Utility --►Provider --►Provider Facility screen for a match of the Billing Provider, Insurance, and Facility. If a match is not found, Intellect looks to the Utility --►Provider --►Provider/ Provider screen for a match of the Billing Provider and Insurance. If a match is not found in either table, Intellect uses the information set up in the Utility --► Provider screen, and then, it is dependent upon Utility --►Insurance --►Insurance <Selection (1/2/3)> for insurance being billed.
FOR LEGACY NUMBERS
• Utility --►Provider --►Provider Facility: Intellect completes the shaded portion of Box 24 J of the CMS 1500 (HCFA) claim form with the entry <HCFA Box 24 J>.
• Utility --►Provider --►Provider Provider: Intellect completes the shaded portion of Box 24 J of the CMS 1500 (HCFA) claim form with the entry <HCFA Box 24 J>.
• Utility --►Provider --►Provider: Intellect completes the shaded portion of Box 24 J of the CMS 1500 (HCFA) claim form with the entry in <HCFA Box 24 J1>, <HCFA Box 24 J2>, or <HCFA Box 24 J3>.
*837 Electronic Claims Submission Equivalent Loop 2310B REF02
NPI NUMBERS
Provider: Intellect completes the lower portion (NPI) of Box 24 J with the entry from Utility --►Provider --►Provider < NPI >
*837 Electronic Claims Submission Equivalent Loop 2310B NM109
If the billing method is clinic (Utility --►Category <Billing Method> = C) the Utility --► Set Up --► Clinic <IRS Number> prints here and the EIN box is marked.
If the billing method is doctor (Utility --►Category <Billing Method> = D), Intellect first looks in the Utility --►Provider --►Provider Facility screen for a match of the Billing Provider, Insurance, and Facility.
• If a match is not found, the program looks to the Utility --►Provider --►Provider/ Provider screen for a match of the Billing Provider and Insurance.
• If a match is not found in either table, Intellect uses the information set up in the Utility --► Provider screen.
Then, depending on the above hierarchy:
Either:
Facility <Tax Id>
Provider/ Provider <Tax Id>
Provider <I.R.S. Id>
prints and an 'X' is marked in the EIN box.
- OR -
The Provider <Social Security No.> field prints, marking the SSN box.
When both <I.R.S. Id> AND <Social Security No.> fields have entries, the <I.R.S. Id> prints here and the EIN box is marked.
*837 Electronic Claims Submission Equivalent Loop 2010AA/AB NM109, NM 108
Box 26 PATIENT'S ACCOUNT NO
This box prints the patient's account number from the Registration --►Regular --►Patient <Patient Account No> field.
*837 Electronic Claims Submission Equivalent Loop 2300 CLM01
If Y has been entered in the Registration --►Regular --►Patient Insurance <Assignment> field, then the Yes box is marked. If N has been entered, then the No box is marked.
If the patient's insurance screen <Assignment> field default was modified at the time of posting charges or through the Charge --►Modify screen, then the Charges --► Charge OR Charges --► Modify <ASI> field entry prints here.
*837 Electronic Claims Submission Equivalent Loop 2300 CLM07
Box 28 TOTAL CHARGE
The sum of all the charges, Boxes 24/1 through 24/6 on the claim form, prints here.
*837 Electronic Claims Submission Equivalent Loop 2300 CLM02
This box prints based on the entry in Utility --► Insurance --► Insurance <Include Payment>. Valid entries are:
Y Prints the total payment posted to the charges in Box 24/1 through 24/6 and the sum of charges minus payments in Box 30.
A Total payment plus adjustment posted to the charges in Box 24/1 through 24/6 and the sum of charges minus payments and adjustments in Box 30.
I Prints the total insurance payments posted to the charges in Box 24/1 through 24/6 and the sum of charges minus insurance payments in Box 30.
B Total Ins payment plus Ins adjustment posted to the charges in Box 24/1through 24/6 and the sum of charges minus Ins payments and Ins adjustments in Box 30.
S Total Ins payment posted to the charges in Box 24/1through 24/6 and the sum of charges minus Ins payments and Ins adjustments in Box 30.
N Prints 0.00. in Box 29 and total charges in Box 30.
*837 Electronic Claims Submission Equivalent Loop 2300 AMT02
The current entry date prints here from Utility --► Set Up --► Clinic <Current Entry Date>.
If Utility --► Insurance --► Insurance <Provider Name (Y/N/X/Z)> = X or Z, the Utility --►Provider <Last Name><First Name> prints here.
*837 Electronic Claims Submission Equivalent Loop 2010AA, 2010 /B AIR 2310 NM1
N3, N4 REF Loop 2010AA, AB,PRV103 BHT03
Intellect prints the Utility --► Facility <Name>, <Address>, <City>, <State>, and <Zip Code> field entries for the code entered when posting Charges --► Charge <Facility> OR Charges --► Modify <Facility>.
This is to be used for other than home or office. For Medicare/Medicaid, leave blank.
Note: When the 'yes' box from Item 20 (Outside Lab) is checked, Item 32 of the claim form must be completed. When billing for purchased diagnostic tests, the provider of service must identify the supplier's name, address, zip code, and NPI in Item 32 of the claim form.
*837 Electronic Claims Submission Equivalent Loop 2310 C/D NM101
2310D NM103 OR 2310C NM109 (TIN) N3 & N4
Intellect prints the Utility --► Facility <NPI>
*837 Electronic Claims Submission Equivalent Loop 2310D NM109
According to the patient's Utility --► Insurance --► Insurance <Selection 1, 2, 3> field setting, enter one of these: Utility --► Facility <Provider 1>, < Provider 2>, or <Provider 3>.
If the charges are related to Mammography, Utility --► Procedure <Mammography> prints here when the Utility --► Procedure <Status> = 'M' is posted.
*837 Electronic Claims Submission Equivalent Loop 2310D REF01 REF02
The Physician's Name, Address, City, State, and Zip Code print as follows:
If the billing method is clinic (Utility --► Set Up --► Parameter <Billing Method> = C, or L with Utility --►Category <Billing Method> = C), physician information prints from the Utility --► Set Up --► Clinic: <Name>, <Address>, <City>, <State>, and <Zip Code> fields.
If the billing method is doctor (Utility --► Set Up --► Parameter <Billing Method> = D, or L with Utility --►Category <Billing Method> = D), physician information prints from the Utility --► Provider --► Provider <Organization Name>, <Address>, <City>, <State>, and <Zip Code> fields.
• If the <Organization Name> field is blank, then this prints the Utility --► Provider --► Provider <Last Name>, <First Name>, <Address>, <City>, <State>, and <Zip Code> fields.
• When both the <Organization Name> and <Last Name><First Name> fields are filled in, the <Organization Name> field prints, along with the <Address>, <City>, <State>, and <Zip Code> fields.
*837 Electronic Claims Submission Equivalent Loop 2010 AA OR 2010 AB NM1, N3, N4 PER
If the billing method is clinic (Utility --► Set Up --► Parameter <Billing Method> = C, or L with Utility --►Category <Billing Method> = C), the billing provider information prints from Utility --► Insurance --► Insurance <Group NPI>.
If the billing method is doctor (Utility --► Set Up --► Parameter <Billing Method> = D, or L with Utility --►Category <Billing Method> = D), Intellect first looks in the Utility --►Provider --►Provider Facility screen for a match of the Billing Provider, Insurance, and Facility.
• If a match is not found, the program looks to the Utility --►Provider --►Provider/ Provider screen for a match of the Billing Provider and Insurance.
• If a match is not found in either table, Intellect uses the information set up in the Utility --► Provider screen.
Based on this hierarchy, one of these prints:
Provider Facility: <Group NPI>
Provider/ Provider: <Group NPI>
Provider: <Group NPI>
*837 Electronic Claims Submission Equivalent Loop 2010AA NM109
After the Dual-use period for NPI expires, this field is only for Atypical Providers.
If the billing method is clinic (Utility --► Set Up --► Parameter <Billing Method> = C, or L with Utility --►Category <Billing Method> = C), this prints:
Utility --► Insurance --► Insurance <Box 33 Type> (the qualifier) followed by
Utility --► Insurance --► Insurance <1500 Form Box 33 Group>
If the billing method is doctor (Utility --► Set Up --► Parameter <Billing Method> = D, or L with Utility --►Category <Billing Method> = D), Intellect first looks in the Utility --►Provider --►Provider Facility screen for a match of the Billing Provider, Insurance, and Facility. If a match is not found, Intellect looks at the Utility --►Provider --►Provider/ Provider screen for a match of the Billing Provider and Insurance.
Based on this hierarchy, one of these prints:
Provider Facility: <HCFA Box33>
Provider/Provider: <HCFA Box33>
If a match is not found in either table, Intellect uses the information set up in the Utility --► Provider screen.
Then, depending on Utility --► Insurance --► Insurance <Selection 1, 2, 3> for insurance being billed, this prints:
Utility --►Provider <HCFA BOX 33.1>
Utility --►Provider <HCFA BOX 33.2>
Utility --►Provider <HCFA BOX 33.2>